Is the Future of mHealth Based on SMS and Inexpensive Mobile Phones?
 James MichielEarlier this month the Finnish mobile phone maker, Nokia, announced that they will be re-releasing an updated version of their legendary 3310 GSM phone. Since it was first released in the early 2000s, the Nokia 3310 has gained a cult following for its incredible durability, long battery life and compact design featuring an internal antenna. Many Europeans and Americans fondly remember the 3310 as their first mobile phone, a device that made meeting up with friends in a crowd easier and a device that provided endless hours of entertainment with the timeless game Snake.
James MichielEarlier this month the Finnish mobile phone maker, Nokia, announced that they will be re-releasing an updated version of their legendary 3310 GSM phone. Since it was first released in the early 2000s, the Nokia 3310 has gained a cult following for its incredible durability, long battery life and compact design featuring an internal antenna. Many Europeans and Americans fondly remember the 3310 as their first mobile phone, a device that made meeting up with friends in a crowd easier and a device that provided endless hours of entertainment with the timeless game Snake.
In the developing world, however, the Nokia 3310 was a lifeline. Owning a reliable, durable communications device that could go days without charging meant that millions of people could connect with relatives and friends in ways they never could before. By the mid-2000s, the spread of phones like the 3310 within the developing world allowed governments and NGOs to reach broad swaths of the population with game-changing speed and efficiency. The use of mobile phones and devices to deliver health services became known as mHealth, or “mobile health,” although the proliferation of mobile devices has been leveraged across many fields including agriculture, governance and finance.
Mobile technology has certainly changed since the 3310 model was released in 2000, as have the ways in which mobile technology is used to reach and deliver services to marginalized populations throughout the developing world. The re-release of this important piece of hardware seems as good a time as any, then, to reflect on the present and future of this growing field.
Moving from SMS to voice and data (and back again)
SMS text messaging has long been the most straightforward and cost-efficient way of directly reaching populations via mobile devices. The Nokia 3310 made huge improvements in user experience with the addition of phonebook functionality and a T9 predictive text keyboard. In recent years, however, the rapid expansion of 2G and 3G availability has combined with increasingly affordable feature phones and smartphones to allow for robust app-based data collection.
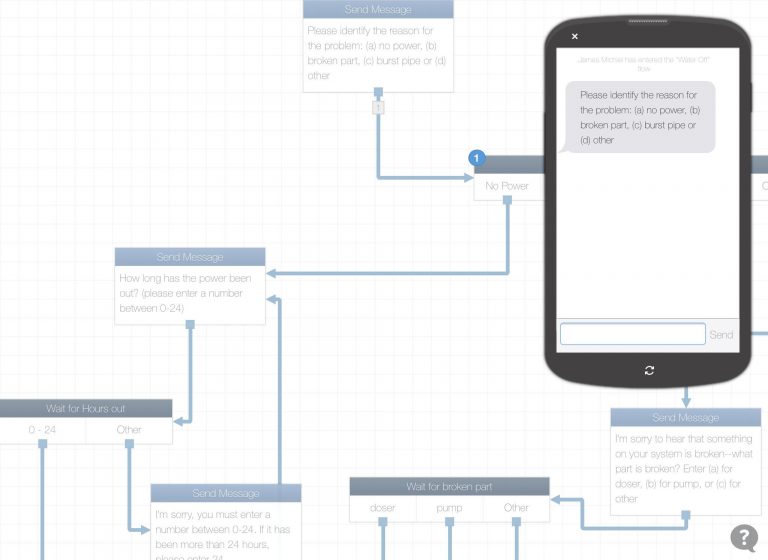 An early prototype of an SMS tool, developed with TextIt, to help healthcare facility staff report water outages. The development team worked closely with program staff to understand the use-case before beginning to build the prototype. (Concept by Marisa Gallegos and James Michel, technical development by Catherine Evans)App-based data collection offers the ability for enumerators to collect GPS and multimedia data, as well as employ complex skip and repeat logic. But these apps also pose technical barriers beyond just finding a reliable data connection—downloading, configuring and using an app for data collection is often a complex process that is not feasible for population-level data collection. While platforms like Open Data Kit (ODK), CommCare and MagPi allow trained enumerators and community health workers to reliably collect a wide range of health data, in most cases these platforms are not feasible to deploy as outward-facing solutions to large, diverse populations. At the other end of the spectrum, SMS platforms like TextIt and Telerivet have evolved to include skip logic and data validation, but there remain limits to what data can be communicated and collected within the confines of a 140-character text message, especially when compared against app-based platforms.
An early prototype of an SMS tool, developed with TextIt, to help healthcare facility staff report water outages. The development team worked closely with program staff to understand the use-case before beginning to build the prototype. (Concept by Marisa Gallegos and James Michel, technical development by Catherine Evans)App-based data collection offers the ability for enumerators to collect GPS and multimedia data, as well as employ complex skip and repeat logic. But these apps also pose technical barriers beyond just finding a reliable data connection—downloading, configuring and using an app for data collection is often a complex process that is not feasible for population-level data collection. While platforms like Open Data Kit (ODK), CommCare and MagPi allow trained enumerators and community health workers to reliably collect a wide range of health data, in most cases these platforms are not feasible to deploy as outward-facing solutions to large, diverse populations. At the other end of the spectrum, SMS platforms like TextIt and Telerivet have evolved to include skip logic and data validation, but there remain limits to what data can be communicated and collected within the confines of a 140-character text message, especially when compared against app-based platforms.
So, how will the gap be bridged between straightforward SMS tools and more complicated but feature-rich apps? In a sense, the two sides have already begun to inch towards each other, and in many ways the pathways for convergence have already been set in motion:
- SMS platforms are becoming more feature-rich. Many have already incorporated Interactive Voice Response (IVR) technology that allow for interactive voice calls, eliminating literacy barriers. Some SMS platforms have also begun moving beyond simple SMS messaging to data-based messaging platforms like WhatsApp, Facebook Messenger and Viber. These data-based messaging platforms allow for more robust interaction and data collection and also have the added benefit of not needing to setup an SMS gateway and/or negotiate shortcodes. Look for further integration of these features into traditional text messaging platforms and interventions in the year(s) to come.
- App-based platforms have traditionally struggled at outward-facing data collection. A notable exception is made possible by Enketo, a web form service that is able to connect to many ODK platforms like Kobo Toolbox and io to allow many (but not all) of the advantages of app-based data collection, including offline data collection, GPS functionality and multimedia, in a browser-based web form.
- Dimagi’s widely-used CommCare platform has begun to bridge this gap more comprehensively than any other single platform. Originally conceived of as a feature-rich fork of ODK (most notably including case functionality which allowed data for a single record to be collected and modified over time), in recent years they have introduced CommCare Messaging (a way to collect data via SMS or IVR using forms created for their app) and more recently, Web Apps (a way to collect data via web forms that mimic their native Android app).
Data and Analysis
There’s a running joke in mHealth that, for many years, organizations that implemented mHealth solutions as part of their programs did so only so that they could use a picture of a locally-based enumerator or CHW holding up a dusty old Nokia 3310 that they had just used to collect some important piece of data. Of course, that’s an incredibly cynical joke, and one that’s mostly untrue. But there is some truth there, not in the cynical sense (I’ve never worked with an organization who just wanted the photo op), but in the sense that many mHealth vendors and practitioners have focused on data collection at the expense of timely analysis and reporting.
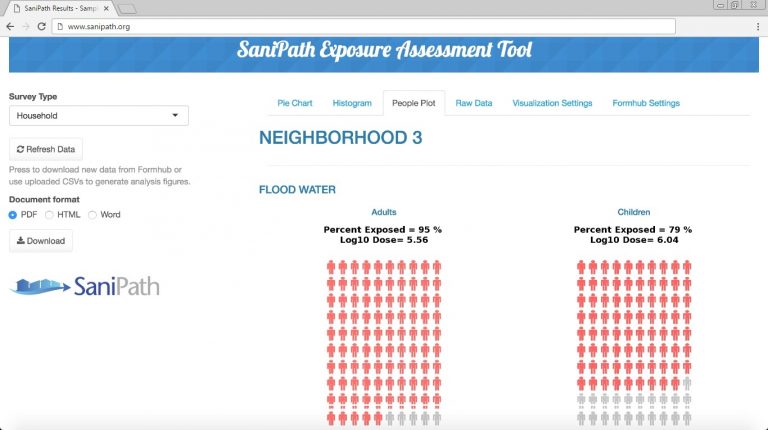 Emory University’s SaniPath Tool collects environmental and behavioral data related to exposure to fecal contamination and then analyzes it to help decision-makers prioritize programs and policies. Data collection is completed using Open Data Kit, with analysis performed in R and displayed using Shiny. This system would not have been possible without custom development, but as the mHealth field matures, we should expect to see an increase in turnkey integration of mobile data collection tools and feature-rich analytic platforms without the need for custom development. (Dashboard by SaniPath’s Yuke Wang)This isn’t to say that mHealth programs have done nothing with the data they have collected. To the contrary, data collected from mHealth interventions are making substantial differences on nearly every continent. Where the gap lies, however, is in the mechanisms for analysis and reporting. While significant work has been undertaken to package analysis and data visualization with mobile data collection, some of the most useful tools have yet to be integrated with data collection:
Emory University’s SaniPath Tool collects environmental and behavioral data related to exposure to fecal contamination and then analyzes it to help decision-makers prioritize programs and policies. Data collection is completed using Open Data Kit, with analysis performed in R and displayed using Shiny. This system would not have been possible without custom development, but as the mHealth field matures, we should expect to see an increase in turnkey integration of mobile data collection tools and feature-rich analytic platforms without the need for custom development. (Dashboard by SaniPath’s Yuke Wang)This isn’t to say that mHealth programs have done nothing with the data they have collected. To the contrary, data collected from mHealth interventions are making substantial differences on nearly every continent. Where the gap lies, however, is in the mechanisms for analysis and reporting. While significant work has been undertaken to package analysis and data visualization with mobile data collection, some of the most useful tools have yet to be integrated with data collection:
- Excel, perhaps the most widely used analysis and reporting tool in mHealth, has long been used to manage and communicate raw data and results. In a sense it’s become a lingua franca for the digital world, especially given its widespread use throughout the developing and developed world. However, it struggles with relational databases and managing longitudinal data sets (in the words of an esteemed colleague, “If you’re trying to develop a relational database in Excel with VBA, you’re doing it wrong”).
- Traditional Business Intelligence platforms like Qlik and Tableau are data platforms built for enterprise use cases that can quickly analyze and visualize data in a way that is both aesthetically pleasing and easy for non-statisticians to understand. Google’s Data Studio is another promising platform that has the potential to offer enterprise-quality analytics and machine learning to a wider audience, beyond those who could traditionally afford/access legacy BI tools.
- Web-based analytic tools, including tools built using open-source languages like R and Python, leverage the cloud for both complex analysis and data visualization. Chief among them is Shiny, an R-based platform that allows R-based analysis to be displayed on user-friendly web-based dashboards.
The over-arching trend here is not that a specific platform or methodology for analyzing mHealth data is emerging as a dominant player, but that the field in general is recognizing that it is simply not enough to collect hard-to-get data. The most successful platforms and programs will will weight collection and analysis equally to achieve the end goal of creating an environment where collected data is used to drive decisions. To that end, platforms like Ona (who have embraced R) and CommCare (with their Report Builder) are ahead of the ball and leading the way to an integrated mHealth ecosystem that prioritizes the use of data equally with the collection of data.
Importance of design
Perhaps the most obvious and important trend in mHealth is that nearly every facet, from development to data collection to analysis, is becoming easier and easier to access for those without formal technical training (and without large technical budgets!). Four or five years ago, it would have been difficult to build an mHealth tool without someone on your team knowing Django, XML, Python or other programming languages. Many, in fact most, of the tools today employ WYSIWYG (What You See Is What You Get) interfaces that allow non-technical users to drag and drop their way to complete mHealth apps without hiring expensive developers or mHealth consultants.
Increased accessibility and lower development costs are undeniably a good thing for ICT4D (Information and Communications Technology for Development) but, to paraphrase a quote from either Voltaire or Spider Man—with the power of cheap and easily accessible mHealth development tools comes the responsibility to design technology-based interventions in a way that is appropriate to the use case (or to recognize when a technical solution is not the right fit). I used to joke with students that the most important skill for an mHealth professional is “how to say NO to someone who thinks they need an app but doesn’t understand their use case.”
For better or worse, we’ve reached a point where there are no gatekeepers to mHealth—anyone who wants to build an app can. It is therefore imperative that the solid fundamentals of mobile development and deliberate, well-planned digital development, are taught and encouraged. I use (and recommend others use) the following resources as a starting point for digital development:
- Principles for Digital Development Created by a consortium of mHealth stakeholders, including funders, NGOs, companies and individuals, the Principles for Digital Development are a set of guidelines for creating digital tools and information systems. While not every principle will apply to every project, and some even seem to contradict themselves (for example, Principle 1: Design With The User, must always be balanced against Principle 3: Design For Scale), I have never worked on a project that did not benefit from a point-by-point discussion of each of these principles.
- Design Kit Human Centered Design is important to any health intervention, but it’s particularly critical for mHealth interventions—not only do you have to ensure that the content is appropriate to the user, but technical capacity and efficacy must also be considered so that the content can be appropriately delivered to the user. Ideo’s Design Kit is a collection of resources, including methods and case studies to ensure that your intervention is not only designed with users in mind, but that the user is at the very center of the design process and that all programmatic and technical decisions are viewed through the lens of how decisions will ultimately affect the end user.
Looking Forward
The future of mHealth is open—open access, open source, open data and open innovation. Never in the history of development have there been so many powerful tools and platforms available to those who have traditionally been marginalized and excluded from the vanguard of technology and innovation. It is imperative, though, that these tools and technologies are used deliberately and efficiently, with an eye towards the end user in a way that ensures long-term sustainability and development.
—
James Michiel is an American public health technologist and writer. He holds an MPH in Epidemiology from the Boston University School of Public Health, is currently a Senior mHealth and Informatics Analyst at Emory University’s Rollins School of Public Health, and also serves as the Senior Tech Guy at NCDFREE. You can connect with him on Twitter at @jamesmichiel
| The Future of mHealth was written by James Michiel and published in PLOS. It is being republished in Open Health News under the terms of the Creative Commons Attribution 4.0 International (CC BY 4.0). The original copy of this article can be found here. |
- Tags:
- 3310 GSM phone
- app-based data collection
- CommCare
- CommCare Messaging
- Commcare platform
- community health workers (CHWs)
- data connection—downloading
- data validation
- data visualization
- data-based messaging platforms
- Design Kit Human Centered Design
- digital development
- Dimagi
- Django
- Enketo
- Excel
- Facebook Messenger
- Google’s Data Studio
- GPS functionality
- health intervention
- ICT4D (Information and Communications Technology for Development)
- interactive voice response (IVR)
- James Michiel
- Kobo Toolbox
- machine learning
- Magpi
- mHealth
- Nokia
- offline data collection
- Open Access. Open Data
- Open Data Kit (ODK)
- Open Innovation
- open source
- Principles for Digital Development
- Python
- Qlik
- quality analytics
- R
- Shiny
- SMS platforms
- SMS text messaging
- Tableau
- Telerivet
- TextIt
- Traditional Business Intelligence platforms
- Viber
- WYSIWYG (What You See Is What You Get) interfaces
- XML
- Login to post comments