Can Providers Continue the Healthcare Continuum Without Medical Apps?
 Thanh TranImagine if banks did not have applications to support mortgage processing! Everything has to be done via a manual process, moving the loan through different verifications and approvals through human coordination. Consumers have to provide bank statements instead of credential approvals to retrieve the information electronically.
Thanh TranImagine if banks did not have applications to support mortgage processing! Everything has to be done via a manual process, moving the loan through different verifications and approvals through human coordination. Consumers have to provide bank statements instead of credential approvals to retrieve the information electronically.
Imagine there is no car loan application! Again, the closing process for a car rolling out of the parking lot takes weeks, instead of hours. What would be the impact to the overall economy?
If air travel would work like healthcare-This humorous video depicts the struggle a passenger would have when making an airline reservation without carrier interoperability. The difference is in healthcare the cost would be much more severe in terms of resources, the impact on patient outcomes, and in a number of occasions, the patient’s life.
HIMSS 2015 attendees traveling to Chicago will experience travel bookings with multiple airlines, hotels and car rentals. The traveler is at the center of all of the services designed to fit their needs. Healthcare does have its own challenges in term of patient privacy, but on the IT perspective the challenges for interoperability and the demand for applications to fulfill the patient’s needs are the same.
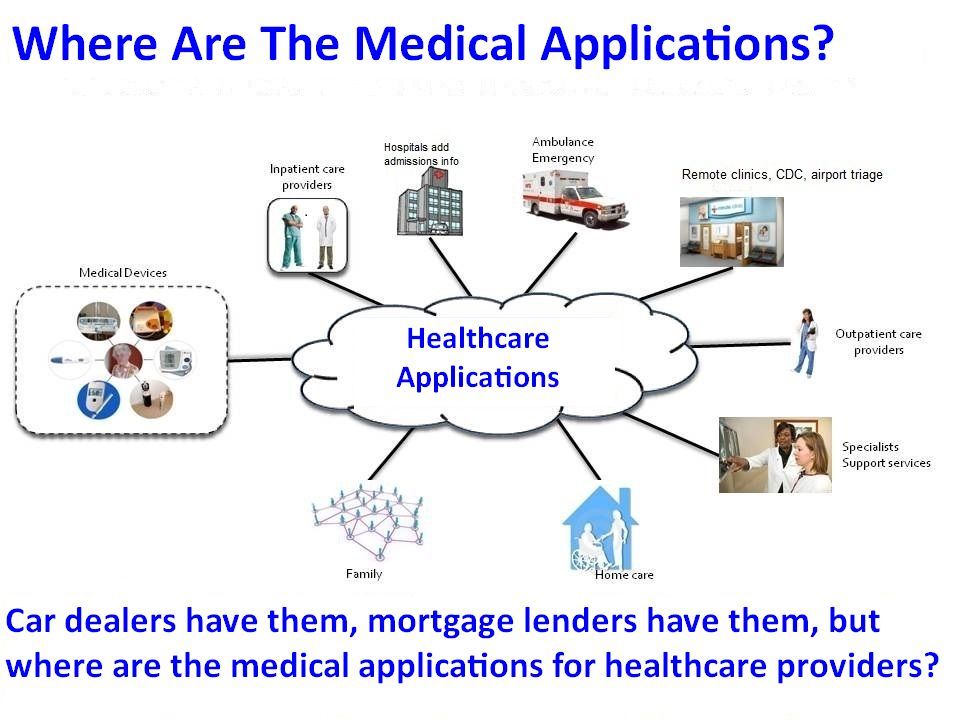
With the HIMSS Conference right around the corner, hospital CIOs and other administrators might want to consider this impact on healthcare as providers ask one simple question: Where are the healthcare applications? Or an even more challenging question; is there a notion of a healthcare application? Is healthcare different from any other vertical industries? Do applications replace physicians or do physicians require applications to address needs in specific care environments?
Why Do We Transform Care Providers into Database Administrators?
EMR and EHR systems are the main engines for the transition of paper to electronic medical records. These systems are designed to record patient medical conditions. They are generic systems with core functionalities similar to a database system.
The former paper medical environment is not just about recording, but supporting manual processes in specific care environments. The most obvious examples are the flow charts built on top of generic EMR and EHR systems. An ICU nurse flow sheet is different than the general visit document from an outpatient clinician. An oncology medical recording is different than a cardiology one. The obvious imbalance on the coverage of an electronic recording system and the expectation of an automated environment is that the paper environment has been overlooked, leading to today’s challenges for providers.
Most of providers’ frustrations have centered on the expectations of a full replacement of the existing paper environment, and further advancements through automation of a generic database oriented EMR or EHR systems. The end result is that providers are presented with a generic database system requiring a database administrator’s skill from its end users. This situation is the same if financial applications do not exist and loan officers are presented with Oracle or Sybase user interfaces to perform their loan processing. Healthcare is much more complicated and impactful since medical errors can impact liability costs and patient lives.
EMR and EHR systems do not cover these diverse processes. They are designed to form a solid base for such processes to be automated, improvements in efficiency, and reduction in costs. The challenge in healthcare today is that the direct end users of such database component should not be care providers.
Healthcare Applications to Address Providers’ Needs in Diverse Care Environments
There is no one-size-fits-all for healthcare providers. They simply need next steps to provide different flow charts for different care environments, often referred as ‘EMR workarounds’. But its description incorrectly assumes that one day an EMR system will provide all needs for providers.
Applications are not ‘database workarounds’. Applications are entities to support automation and to support end user efficiencies. Applications cannot exist without a database component and are designed to serve end users with a set of specific needs, including ease of use.
As noted previously, loan officers are trained to review and approve loan applications. They are not trained as database administrators tasked with navigating different database systems from different vendors. Care providers are no different. They are trained to provide patient care in their specific environment. They need specific tools such as healthcare applications to do their jobs, but they don’t have them. So where are the healthcare applications to support them?
Roadblocks for Application Developers—Costly, Complicated Infrastructures
Major healthcare facilities with significant IT budgets such as Kaiser, Mayo, Cleveland Clinic and others have the ability to provide customized environments for their care providers—EMR workarounds. While these customized solutions are relatively simple, they are very specific to one environment. They are also costly to develop, adaption to a new environment is challenging and only the big healthcare organizations can afford them, not a community hospital. The complexity begins with lack of EHR interoperability, but it is not the only difficulty.
Most care environments require the support for a messaging or notification service, a polling service to trigger notification if a patient’s condition changes. Such services are common and can be shared among healthcare applications. With most of these common services pre-developed, applications developers can focus on innovating solutions for providers to improve patient outcomes and reduce operational costs.
Healthcare needs healthcare applications to address providers’ needs in diverse care environment. We must remove the roadblock so that application developers can focus on healthcare innovation. It is the only way to improve patient outcomes, reduce costs and increase providers’ efficiency and scalability. Only healthcare applications would address care collaboration, patient engagement, and all the challenges being long discussed, but no solutions exist in today’s healthcare industry.
Consumer and Patient Centric Model
Dell Computer’s success has been based on a consumer centric model for computer purchasers. This model changed how computers were built, delivered and supported. Dell’s computers are designed based on that model, beginning with part inventory, hardware designs, manufacturing, and delivery through to customer support.
This process has propelled Dell Computer to a leadership position, but above all, changed the consumer expectation. From the consumer perspective, Dell represents applications aiming at improving personal computer purchases along with all the supporting capabilities.
In healthcare, we often talk about a patient centric model. Its challenges begin with a lack of EHR interoperability. Each patient has their own set of healthcare facilities where there records are kept. These records are supported by different EHR systems from different EHR vendors.
This is where the patient medical information flow begins, but it does not stop there. Each patient has different healthcare needs from different care environments where care providers’ collaborations are different. Each of these environments requires different processes to focus on patient care.
Here are two examples of healthcare’s current state in terms of a patient centric model.
- A patient is discharged from a hospital after a surgery. The discharge report instructs that the patient checks in to a wound care center for follow-up. In today’s environment, there is no support for ‘patient follow-up’ and ‘anticipation of potential healthcare problems’. What if the patient does not check in to the wound care center? What would be the patient’s challenge to get to the wound care center? Hospitals and clinics are incented to provide such follow-ups and hand-offs between healthcare facilities, but there is no application or mechanism to support its efforts. At best, it would be a manual, human intensive engagement.
- A patient checks in to emergency room for a bone fracture. The emergency room physician deems that a general doctor can handle the treatment the next day. An x-ray is taken and some basic check-ins are done at the ER. The patient shows up at the general doctor’s office. What are today’s capabilities for such seamless hand-offs from an ER to a general physician?
These are simple examples of a patient centric model. There are huge benefits for such seamless engagements as noted in the CMS care guideline.
Addressing Healthcare Based on a Patient Centric Model
A patient centric model needs to be supported by applications. Healthcare applications are required to support a seamless process across multiple healthcare facilities. Such applications need the support of a seamless medical information flow, personalized on a per-patient case like an airline or a bank has.
Healthcare applications are missing. Health IT organizations cannot fulfill their support to medical professionals. Patient centric models have been a theory, or at best, supported by manual processes, exposed to human errors. Healthcare application availability has been limited by the healthcare infrastructure and the lack of common services mostly available for its siblings in other vertical markets described earlier.
Not Just Generic Middleware, But Healthcare Middleware
Healthcare applications face different challenges than their counterpart in consumer applications. They are not designed to replace providers or to improve the efficiency and scalability of providers. EMR and EHR systems have common characteristics with a database system, but they are designed for healthcare. In other words, healthcare needs its own stack.
Healthcare middleware must address all the common services required to support application development. Having a set of APIs access EMR and EHR systems is the starting point, but not the complete solution. Messaging, workflow, rule engine services, and more must be part of a middleware solution. Its footprint must be lightweight and cost efficient so that it can be embedded with the applications.
The real healthcare challenge is addressing the missing healthcare applications in support of a diverse care environment. Our efforts must align to inspire developers in addressing providers’ needs. It will be healthcare applications that will evolve healthcare to the next level.
However, healthcare 2.0 organizations like Zoeticx are beginning to make a difference. Zoeticx uses middleware technology to integrate with EHRs to overcome their lack of support for interoperability. The Zoeticx Patient-Clarity platform is patient-centric healthcare software that uses middleware to enable patient medical information to flow from diverse EHR sources, presenting patient medical data across the care continuum, transforming passive patient medical data into actionable information.
Its Health Oriented Architecture (HOA) leverages IT advancements from vertical market platforms such as finance. This architecture also enables it to readily support the next generation of healthcare applications which can easily be built by health record app developers through its open API.
- Tags:
- database workarounds
- electronic health records (EHRs)
- electronic medical records (EMRs)
- EMR workarounds
- Health Oriented Architecture (HOA)
- healthcare 2.0 organizations
- healthcare applications
- healthcare continuum
- healthcare middleware
- HIMSS 2015
- lack of EHR interoperability
- messaging
- patient centric model
- patient medical conditions
- patient medical data
- patient medical information
- patient-centric healthcare software
- rule engine services
- seamless medical information flow
- Thanh Tran
- workflow
- Zoeticx
- Zoeticx Patient-Clarity platform
- Login to post comments