The Time to Stop Giving Antibiotics to Cows, Pigs, and Chickens Is Now
Antibiotic resistance has been blamed for at least 2 million illnesses and 23,000 deaths in the US. Researchers are especially concerned about the widespread use of antibiotics in raising cattle, pigs, and other animals for food production. The drugs help the animals bulk up, which boosts their value, but experts warn that they can also promote antibiotic resistance. I’ve asked two guest authors, Josh Bloom and Dr. David Shlaes of the American Council on Science and Health, to share their insights on this issue. They warn that more needs to be done to curb the use of antibiotics in food-producing animals.
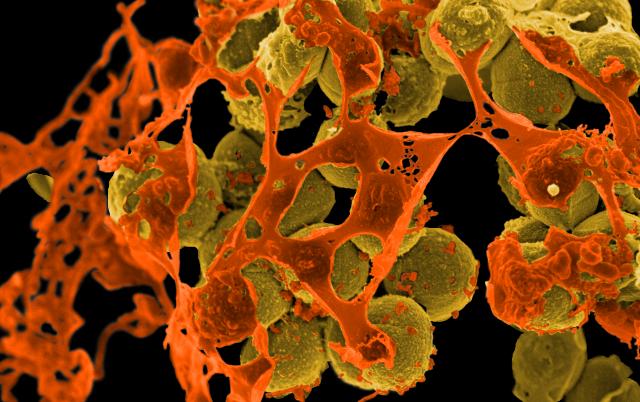 Scanning electron micrograph of methicillin-resistant Staphylococcus aureus (MRSA, brown) surrounded by cellular debris. MRSA resists treatment with many antibiotics. Credit- NIAID, CC-BY-2.0, FlickrBy Josh Bloom and Dr. David Shlaes
Scanning electron micrograph of methicillin-resistant Staphylococcus aureus (MRSA, brown) surrounded by cellular debris. MRSA resists treatment with many antibiotics. Credit- NIAID, CC-BY-2.0, FlickrBy Josh Bloom and Dr. David Shlaes
The recent discovery in China of a new gene found in bacteria in both pigs and humans should both infuriate and terrify the public health community. The gene is called mcr-1, and it is responsible for a new, specific type of bacterial antibiotic resistance — precisely the last thing that the world needs at a time when many antibiotics, which once easily cured infections, have stopped working. Yet, it would be wrong to lay all of the blame on China since they are not alone in adding antibiotics to feed, a long-used practice, including in the US despite the considerable body of scientific evidence that tells us that this is a very bad idea. Adding antibiotics to animal feed makes the animals grow faster but the practice has also clearly paved the way for the formation of mcr-1.
Bacteria have many tricks up their sleeves. One is the ability to transfer genetic information via plasmids — small circular pieces of DNA that are separate from the normal DNA of the bug — which easily carry genes from one bacterium to another, even if the two are unrelated. In 2008, a scary superbug called NDM-1, short for New Delhi Metallo-beta-lactamase-1, was discovered in New Delhi (hence the name) that was resistant to almost every antibiotic. The one drug we have left that still works against such strains is called polymyxin, an antibiotic that is toxic and so rarely used that many physicians don’t even know how to administer it correctly.
But, sometimes it is the only choice, since it is the last remaining weapon in the antibacterial arsenal. One strain of NDM-1 bacteria is carbapenem-resistant Enterobacteriaceae (CRE), which is so lethal that roughly half of infected hospital patients will die — an alarmingly high mortality rate. A scenario in which both of these genes are operating in the same germ is chilling. For example, if a CRE strain also acquires the mcr-1 polymyxin gene, it becomes virtually untreatable. Although such strains are still uncommon, they are spreading. The polymyxin resistance gene is now found in bacteria collected from 15 percent of samples of all raw meat, 21 percent of pigs, and 1 percent of samples from hospital patients with infections. The gene has already been found outside of China, as well...
- Login to post comments