Closing the Referral Problem in Distributed Care Networks
 Dr. Peter S. TrippettThere have been any number of people and companies working tirelessly to solve healthcare's interoperability challenges. Hospitals, EHR software companies, Health Information Exchanges (HIEs), Federal and State governments, payers, and others have developed, tested, and implemented many in-house or vendor-built solutions to try to clear this hurdle.
Dr. Peter S. TrippettThere have been any number of people and companies working tirelessly to solve healthcare's interoperability challenges. Hospitals, EHR software companies, Health Information Exchanges (HIEs), Federal and State governments, payers, and others have developed, tested, and implemented many in-house or vendor-built solutions to try to clear this hurdle.
Recently, consumer technology vendors and patient-centered innovation programs have begun to make significant strides on directly expanding patients access to their own records. This is great news for patients, but when I am a patient, I also want my doctors and other caregivers to be able to communicate about me when needed. So, making me responsible for stewarding pieces of my record between them doesn't solve the challenge. Especially if I have received care in three or four different places or worse yet, become incapacitated.
Why haven't current efforts yielded greater interoperability?
Because in large part, they have relied on pre-planned, point-to-point integration or members-only sharing collaboratives. While each of these can be effective, they inevitably exclude significant portions of a broad network of affiliates, health workers and community healthcare organizations with whom they collaborate (primary care, specialty care, SNF, etc.).
Most hospitals and health systems operate with a distributed care network, which has a combination of:
- In-network ambulatory & specialty practices running the Hospital-approved EHR
- In-network ambulatory & specialty practices running another EHR, and
- Out-of-network ambulatory & specialty practices running any of hundreds of different EHRs
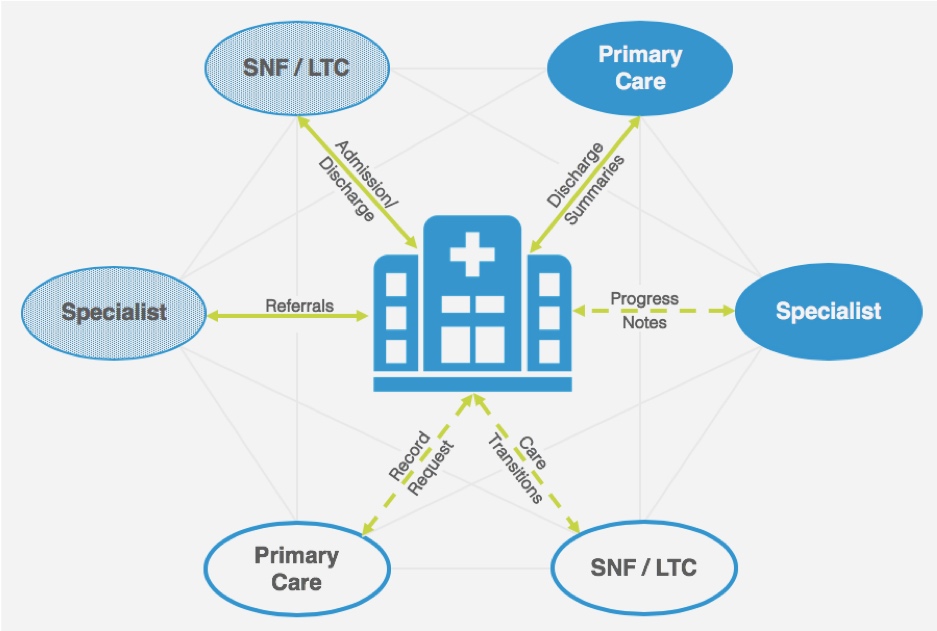 The providers using the dominant Hospital EHR (shown in dark blue in the diagram) tend to experience good medical record sharing and information exchange, clinical data availability in both directions during care transitions, and decent analytics capabilities across both inpatient and outpatient data.
The providers using the dominant Hospital EHR (shown in dark blue in the diagram) tend to experience good medical record sharing and information exchange, clinical data availability in both directions during care transitions, and decent analytics capabilities across both inpatient and outpatient data.
In many cases, in-network practices running another EHR (in light blue) start to run into trouble. Some in this group may leverage protocols and processes (Fax, Direct, HIE, EHR portals) to meet a portion of their requirements or switch between two EHR interfaces to get things done. This is not ideal since it limits the sharing of structured data or may rely on "pulling" patient data from a portal.
For the third category (in white), there tend to be two out-of-network practice types, neither of which is formally aligned with the hospital:
- Practices from whom the Hospital/Health system regularly receives patients or sends referrals/discharges. Services such as ADT alerts via the HIE may be helpful for these if the recipient has joined the same HIE.
- Practices that are not a part of the regular, local/regional care community. These may include out-of-town practices of a traveling patient or other facilities and practices that are involved in a patient's care, such as a specialty cancer treatment center.
In these cases, most admissions, discharges and referrals are manual, delivered through paper or fax, and are painful at both ends.
With the realities of a distributed physician network in mind, the industry has a lot to gain by re-thinking its reliance on point-to-point integration, and instead use a wide variety of standards for exchanging health records including Direct, XDS, XDR and FHIR along with the primary standards for the health records themselves including current and legacy CDAs, C-CDAs and FHIR records. By layering this with additional tools such as a clinician directory and cloud-based secure messaging that transcend enterprises to expand reach, all providers would be better connected and less reliant on the EHR vendor they use or what HIEs or other sharing networks they have joined.
And even when the outside provider is part of the same HIE or sharing network, there are commonly important components of a referral or transition of care workflow that are not available via those networks. Simple things like clinical notes, referral or discharge summaries, and complex and very large items such as EEGs or MRIs, photographs, or scheduling information are all common challenges. And messaging is rarely connected to medical record sharing in ways that makes asking questions about a patient's record of another provider easy.
Furthermore, as we build a better understanding of how social determinants of health (SDoH) impact outcomes and engage tertiary members of the care team (such as public health workers who operate outside an EHR), we should continue to build on the "core" acute care communications capabilities and ensure the right person can be included at the right time, regardless of the clinical role they play in a patient's care.
careMESH is the only service provider that guarantees 100% digital delivery of all referrals and care transitions (including both medical records and messages) to any healthcare provider nationwide. This is ideal for hospitals sending discharge summaries and patient records to far-flung PCPs, for small local providers on different EHRs, and everyone in between.
We invite you to visit us at HIMSS19 Booth 9000-71 in Orlando, FL on February 12th - 14th or drop me an email anytime.
- Tags:
- acute care communications capabilities
- careMESH
- clinical data availability
- clinician directory
- cloud-based secure messaging
- distributed physician network
- health information exchanges (HIEs)
- HIMSS19
- medical information exchange
- medical record sharing
- patient-centered innovation programs
- Peter Tippett
- public health workers
- social determinants of health (SDOH)
- Login to post comments