“WE ARE” Data-driven Social Determinants of Health for Life
 Doug GoldsteinWho are you? Today the data knows! DataStreams are being created by each of our mobile and Internet-connected devices moment by moment each and every day. In fact, 90% of all data created in the history of humankind has been created in the last few years. We are talking in excess of two quintillion bytes of data a day being generated. A quintillion is a billion, billion; the data generated by our interactions with the Web, Twitter®, Amazon®, every Google® search, text message, photo taken, command sent to Alexa and all our other actions recorded as digital data is the number TWO followed by 18 zeros! The challenge in healthcare today is knowing the elements and characteristics of the DataStreams as they relate to the overall Determinants of Health. The goal is to ethically and legally harness data to develop new products and services that can improve health quality and lower costs, while delivering value and profitability within sustainable organizations.
Doug GoldsteinWho are you? Today the data knows! DataStreams are being created by each of our mobile and Internet-connected devices moment by moment each and every day. In fact, 90% of all data created in the history of humankind has been created in the last few years. We are talking in excess of two quintillion bytes of data a day being generated. A quintillion is a billion, billion; the data generated by our interactions with the Web, Twitter®, Amazon®, every Google® search, text message, photo taken, command sent to Alexa and all our other actions recorded as digital data is the number TWO followed by 18 zeros! The challenge in healthcare today is knowing the elements and characteristics of the DataStreams as they relate to the overall Determinants of Health. The goal is to ethically and legally harness data to develop new products and services that can improve health quality and lower costs, while delivering value and profitability within sustainable organizations.
There are four broad "Determinants of Health" zones influencing our longevity, quality of life and total costs of health care. These zones include:
- Multi-omic, biological analyses including our genetic, proteomic, microbiome and other "omic" profiles
- Social Determinants of Health (SDoH) including economic, social and environment factors
- Medical care, which is actual clinical care delivered and recorded, and
- Health Behaviors including a person's daily behaviors (e.g., activity, nutrition, sleep and coping skills).
The percentages in Figure 1 are a synthesis of the authors' analyses of multiple information sources. The key observation is that our social, environmental and individual health behavior factors impact up to 70% on the total cost and outcomes of care within the industry.
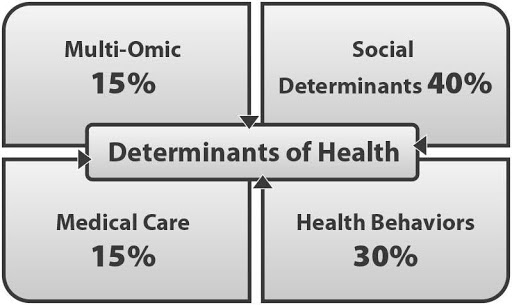 Figure 1. Determinants of HealthIn our digital world there are six primary DataStreams that can be applied to address health challenges:
Figure 1. Determinants of HealthIn our digital world there are six primary DataStreams that can be applied to address health challenges:- Social Data
- Multi-omic (biological) Data;
- Medical Data;
- Financial Transactions Data;
- Digital data (from wearables, Internet-connected devices (e.g., IoT), mobile app use, etc., and
- Public sources of data (e.g., census data, neighborhood crime and real estate reports, public health data and more).
All of these six DataStreams are profiled in this article, with additional focus on health-related behaviors and data-driven SDoH factors. In today's world, healthcare decisions and treatments can be customized with the help of the data being created and tracked by nearly every one of us every minute of every day.
The "WE ARE" DataStream
Our focus includes understanding the many SDoH-related dimensions, and extracting targeted, relevant data points from the growing six DataStreams in productive ways that were not possible a few years ago. "WE ARE" is an easy way to understand all the underlying dimensions involved in analyzing the total impacts of SDoH factors. In the past the adage was "you are what you eat". Today it is "we are the data we generate"! The summary of "WE ARE" below is expanded in greater detail throughout the article.
 Figure 2. “WE ARE” Data-driven Social Determinants of Health
Figure 2. “WE ARE” Data-driven Social Determinants of Health
- W = Work - A person and their family employment circumstances can influence overall stress levels, physical impact on the body (excessive sitting or heavy, manual labor), mental health and overall lifestyle.
- E = Environment Where you live determines the quality of water, air and food available to you. The place where you grew up impacts early childhood development and the habits impacting your adult life.
- A = Abilities and Addictions - Each of us has created a positive set of "abilities" or skills that help manage activities of daily living. And each of us can have negative "addictions" (e.g., drug, food, Internet and others), and/or other forms of negative behaviors.
- R = Relationships - People with sustained, positive relationships have lower mortality rates. Loneliness and isolation are proven to negatively impact mental health and overall health status. The "Relationships" element includes the cultural context and social status surrounding us.
- E = Education - A person's education level strongly influences employment opportunities and social standing. Another component within the education category is health literacy, which is defined as the ability to understand and manage both the medical and financial complexities of our healthcare system.
The imperative is to understand the SDoH dimensions and the underlying DataStreams available to our organizations to improve processes and create new solutions. This requires the wise application of data science, technology, processes and human ingenuity to develop solutions that deliver value and improve the human condition.
Data Everywhere. Data Defines and Drives Our Lives.
By 2019 it is estimated that 67% of the world's population will have a mobile phone1 . Our actions everyday create a vast number of digital data points recording our actions through the mobile and Internet-connected devices that digitize our lives. These digitized data trails are being bought, sold and traded every day. Every credit card purchase, Internet search, use of a mobile app and/or voice command to our virtual agents (e.g., Alexa, Siri or Cortana) is transformed into digital data that is analyzed and stored for future use by you or others. All of your personal data points are tracked and sold multiple times and become part of your "digital data biography". This biography of "You" (or pieces of it) is stored across the databases of Google®, Apple®, Amazon®, Facebook®, mobile app creators and thousands of companies including data brokers.
The data explosion will continue with over 200 billion IoT devices by 2020 sensing, tracking, and predicting our every action, based on Intel Corporation analysis. All of these connected devices generate a true "tsunami of data" to be bought and sold to accelerate consumer purchasing behavior, but can also be harnessed for health and wellness purposes. The health industry's challenge is how to use all of this collective and individual data to improve individual,
family, and community health status, while understanding and abiding by data privacy and security requirements and value-based boundaries.
New data is generated every nanosecond from all of our collective actions, and the key challenges health leaders must address are:
- Data leadership; specifically, the growing talent gap is becoming more critical
- Data explosion accelerating
- Data complexity expanding, and
- Data velocity increasing.
It is a general tenet that most people seek overall health and well-being. We spend our lives seeking good food (sometimes too much of that), supportive friends and family, clean water, fulfilling jobs and a sustainable world that we can all live in. Then illness strikes and changes the picture. The tenacity is for people and our health community as a whole to look for the quick fix in a pill or medical treatment.
Upwards of 60 to 70% of the total cost of health care and outcomes improvement are related to SDoH factors and individual behaviors. The industry must continue the focused shift from reactive to preventive care through the use and analysis of new data sources throughout the entire health ecosystem. Successful organizations addressing this shift will incorporate strategic leadership, big data capabilities and infrastructure to ethically ingest and transform key data elements. These new sources of data elements must also be used intelligently to create and improve ways to structure clinical care and care management processes, including the use of non-traditional care supports (e.g. nutrition services, home health aides, transportation services).
DataStreams to Harness for Data-driven SDoH Solutions
Are we healthy or not? And if not, how do we get to a culture of health? This is a complex question influenced by not only the "WE ARE" SDoH DataStreams, but also the five other streams fed by mobile and Internet-connected devices. All of which have big impacts on the health and well-being of individuals, families and populations.
Data Streams to Innovate Solutions
Are we healthy or not? The data knows! All the DataStreams are increasingly fed by larger and larger digital data sourcing from mobile and billions of Internet-connected devices. Each of the six DataStreams have data elements that can be captured and analyzed to improve interventions and create new innovation solutions.
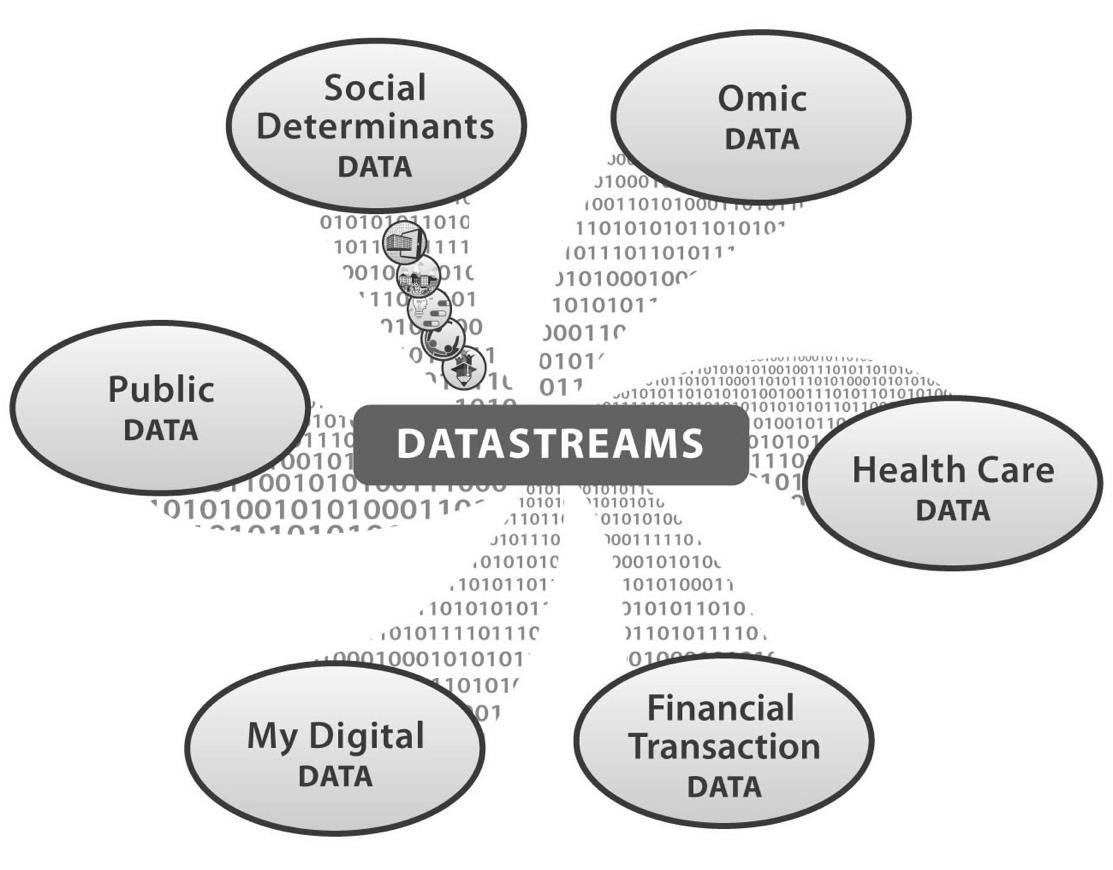 Figure 3. Six Data Streams Driving Determinants of Health
Figure 3. Six Data Streams Driving Determinants of Health
#1. "WE ARE" Social Determinants Data - The "WE ARE" SDoH DataStream is composed of dimensions of: Work - Environment - Abilities/Addictions - Relationships - Education. These five sub-dimensions span the conditions, relationships and environments in which people are born, live, work, and age as individuals, families within their community. It is estimated that SDoH factors impact 40% of our health status and costs. In addition, SDoH factors provide the foundation that leads to health behaviors, which account for another 30% of overall health, functioning and quality-of-life factors. Data from all of these DataStreams can catalyze care-related insights in addition to new product and service development. Data being generated from the expanding universe of mobile, wearable and IoT devices are a vital source for improving the health of a community. The U.S. Centers for Disease Control (CDC) has a series of tools and resources that include data sources and references. Initiatives to improve health can harvest data on SDoH factors from the CDC 2. Exploring this link reveals many valuable data sources such as chronic disease indicators, state-and metropolitan-level data, an interactive heart disease and stoke atlas, information from the National Environmental Public Health Tracking Network, Social Vulnerability Index and much more. These sources provide both resources and tools to explore and profile the data in a form that can be useful to many health industry stakeholders.
Another powerful source of data for the "We Are" DataStreams is the CDC's Data Set Directory3.This is a comprehensive guide to public data sources covering the following: Economy; Employment, Education; Political; Environmental; Housing; Medical; Government; Public Health; Psychological; Behavioral and Transport. There continues to be a U.S. industry-wide effort to "liberate" health-related data wherever it lives to support new product and service development that can improve health through a combination of scientific approaches, SDoH data analysis, and personal behavior modification approaches. Recently announced initiatives from the U.S. Centers for Medicare and Medicaid Services (CMS)4, including MyHealthEData and Blue Button 2.0, aim to give consumers direct access to their clinical and health claims data, including access to this data from mobile apps. It is anticipated this expanded access to data can better empower consumers to better understand their total picture of health, while also incentivizing health IT developers to develop new solutions that can place this information into meaningful and actionable context.
#2. Multi-Omic (Biological) Data - is a new, dynamic field that is rapidly expanding as science and technology learn to profile and analyze complex interactions between the "-omics" in our bodies. This involves gathering biological samples and analyzing multiple -omic datasets including genomic, proteomic, microbiomic, metabolomics and pharmagenomics. The objective is to find "actionable" findings. This could be as simple as a pharmagenomic test that determines how fast someone metabolizes a certain class of drugs, or as complex as profiling a cancer tumor with genetics and proteome factors. Single and multi-omic analyses involves big data to detect multiple data point associations and determine what is actionable or not. The U.S. National Institutes of Health (NIH) "All of Us" precision medicine initiative will gather multi-omic data along with other DataStreams, such a person's digital data (e.g., wearables, mobile apps and more) on one million Americans. There are many health leaders entering and expanding their multi-omic programs. Some examples include:
- Inova Health System and the University of Virginia's efforts to build the Global Genomic and Bioinformatics Institute
- Geisinger Health's expansion of its precision health program with the launch of the Geisinger National Precision Health Initiative, and
- the U.S. Veterans Administration's Million Veterans Program (MVP), where they are building an -omic repository and database based on one million veterans.
#3. Health Care Data - represents data obtained from clinical sources, including electronic health records (EHRs), home health records, care management plans and other health and medical sources. Many health organizations have developed sophisticated enterprise data warehouses, while others are implementing advanced data mining, analyses and visualization technologies, combined with processes and tools to ensure privacy and security compliance. It is important to note that EHRs are historical records and not designed to be real-time, dynamic measures of health signals such as vital signs, weight, etc. Meanwhile, health organizations are challenged to meet the ambitious data exchange targets of CMS' Meaningful Use program, while they also trying to structure enterprise infrastructure to meet quality reporting requirements, including CMS' Star ratings. The idea of establishing the role of a Chief Data Officer, combined with role authority, budget and C-suite reporting relationships, is just now entering into the structure of innovative organizations. Nevertheless, many legal, regulatory and business model issues affect the challenges of complete and/or targeted data integration.
#4. Financial Transaction Data - Every medical episode results in data being generated from the transaction, and these episodes have medical elements that drive total financial costs. Every part of the medical episode has multiple data angles, such as the physician fee, facility fee, drug prescription and many data points along the continuum of health care. Data from inside the health system includes mostly claims-related data from services and products, such as a prescription given and filled. Data from outside the health care system includes a wide array of consumer purchases, including groceries, over-the-counter health supplies, and goods and services not covered by insurance (and therefore not tracked within clinical or financial health data repositories). Clinical data is very complex and is used for multiple functions such as care management processes, quality measure reporting and financial reimbursement. Claims data is less dimensional than clinical data, but also offers fewer insights relative to patient behavior because it is narrow in scope by definition.
#5. My Digital Data - Billions of IoT-connected devices, including Fitbits®, Apple®, Watches, mobile smart phones, mobile apps, voice agents (e.g., Siri, Alexa, Cortana, etc.) and many other devices are generating digital data all of the time. In health care we often call this "User or Participant Generated Data". All or parts of this DataStream category can be used by an individual to improve fitness levels by tracking intentional and unintentional physical activities, and relating this information to diet, weight and other health measures. This data relationship can be performed for every disease category. Asthma inhalers now have sensors that track the amount of rescue medication versus maintenance medication doses, while insulin injector pens can track dosage and share it with the patient directly and their care team. Digital Data from devices, mobile apps, cameras and other devices are increasingly being connected to the other DataStreams, such as a genomic profile, in ways that can help an individual know what drug to take or not to take, and how to optimize recovery processes following a surgery.
In many cases the Digital Data DataStream is accessible to the individual directly. However, there are significant, passive data streams being generated by the sensors in a mobile device, including accelerometer, GPS, altimeter, gravity, Bluetooth, camera, mobile apps, and virtual agents. All of these sources represent a wealth of data to be bought, sold and harnessed for positive health purposes. Like any tool where data is passively moved from an app, sensor or virtual agent, the collective DataStream can be used for both positive or negative purposes.
#6. Public Data - There are vast stores of public data that can be used for healthcare purposes, and many of these sources are available from U.S. government agencies. The Public DataStream includes geographic data, regional financial data and individual financial data; neighborhood data such as access to transportation, nutrition, housing type, income levels and crime rates; and individual purchasing behavior as captured by credit cards, store loyalty programs many others. Here is sampling of available sources which are just the tip of the proverbial iceberg:
- Tour Data.gov- a federal government effort to make all of its data available freely online. It is a work in progress.
- Examine Healthdata.gov, which features U.S. healthcare data including claim-level Medicare data, epidemiology and population statistics for the last 125 years.
- Explore public data sets on the 1000 Human Genome Project (one of the most comprehensive database of human genetic information), and other data wonders at Amazon Web Services public datasets5.
- Gain insights from the Pew Research Center, which offers raw data from its fascinating research into American life, including The Internet and American Life Project.
- And don't forget to check out Google Public Data Explorer6. This is a great tool to identify and visualize data because it provides charts and maps that animate over time illustrating the changes in the world of the datasets you have selected.
To transform health care from a reactive, sick care system to a proactive, preventive system, we must understand the six DataStreams to energize effective, new solutions to improve the health of individuals, families, communities and populations.
"WE ARE - Data-driven SDoH Influencing Medical Costs and Outcomes
The study of SDoH factors goes back at least 40 years to the 1979 U.S. Surgeon General's Report: "Healthy People"7.This same study was consequently updated in 1990, 2000 and 2010. The Henry J. Kaiser Foundation has also been active in research in this area. The Accountable Care Act (ACA) and the shift to value-based reimbursement accelerated the research and applications of SDoH within the population health field. As a result of our industry innovation work, we have coined the term "WE ARE" to describe the next generation of data-driven SDoH components.
- W = Work. A person's and/or family's employment circumstances can influence overall stress levels, physical impact on the body (excessive sitting vs heavy, manual labor), mental health and overall lifestyle. Income level in the past, present and future is a critical factor impacting lifestyle factors ranging from diet quality, total exercise level, and day-to-day stressors experienced. Overall financial instability results in higher levels of stress. Lower and/or unstable income impacts nutrition levels and could tend to increase the likelihood of chronic conditions such as diabetes, obesity, hypertension and more. Individuals in uncertain employment situations are more likely to have a lower quality of life and less access to essential healthcare services. This kind of instability tends to limit access to quality food, housing, reliable transportation and stable employment. Numerous studies using government, demographic and income distribution data have correlated that disadvantaged households tend to have poorer health status than higher income communities.
- E = Environment. Environment is composed of the following components: 1) physical environment of the home, specific geographic area, climate, air quality and other related factors; and 2) social strata of the household, schools and overall community-wide social adhesion. Where you live determines the quality of water, air and food available. The place where you grew up impacts early childhood development and the abilities to work and socialize as an adult. Stress levels arise from both the physical and social environment. Continued exposure to high levels of stress has been repeatedly associated with a broad spectrum of negative health outcomes.
An example of using environmental data is a concept called "hotspotting", where super-utilizers are identified through a combination of social, health and environmental data. One example of hotspotting includes an examination of a specific senior living facility with an excessive number of falls resulting in excessive hospital admissions for the residents. The practice of hotspotting in this scenario would analyze SDoH-related data to discover the super-utilizer(s) (e.g. frequent fallers), and address the problem by organizing health, social services and other cross agency resources to remedy all of the conditions leading to unsafe factors and related falls. These factors could include housing quality, mental health, substance abuse, emotional support and more. Aggregated data can provide the clues on where to focus scarce resources, whether it be the addition of more home care aide support, facility improvements, additional nursing staff and/or remote health monitoring technology.
- A = Abilities and Addictions. Each of us has evolved a positive set of "Abilities" or skills that help manage activities of daily living (ADL). These Abilities are a result of an intersection of forces across all the SDoH dimensions. In addition, the abilities individuals have developed will determine the type and stability of their employment, which has significant implications for nutrition, security and stress levels. Abilities also determine an individual's total contribution to citizenship and overall community welfare.
Humans are creatures of habit. Along with the positive abilities each person has developed, there is also a set of negative "addictions" that are formed, which could be mild or serious and includes smoking, drinking, drug abuse, gambling, social isolation and other forms of negative behaviors. Many people strive for moderation and one or more negative addictions could arise after a significant traumatic life event; this negative behavior can then become ingrained into one's lifestyle. Numerous studies have shown that negative addictions have a direct correlation to poorer health status and various mental health conditions. Now for the first time in history there is a universe of DataStreams that can be tapped to understand this dynamic and interaction between abilities and addictions.
- R = Relationships. The "Relationships" dimension includes the cultural context and social status surrounding us. Relationships layers include a person's relationships with their significant other, with family and friends, with associates at work, with the community they live and the overall culture. In healthcare there are studies illustrating that inequalities in population health status are related to inequalities in social status. In the U.S., social status is driven in part by birth and ethnic origins, but occupation (blue collar vs. white collar) is also a primary influencer. American society has provided options for upward mobility. This is not to say that diversity issues don't exist within the culture. Humans are tribal animals based on our evolution, and social adhesion within a community or tribe is rooted in both our genetics and environmental circumstances. Studies have shown that socially isolated adults have lower qualities of physical and mental health. Numerous studies have shown that people with sustained relationships have lower mortality rates, improved cardiac health and longevity.
In the data-driven digital age, very important "relationship" layers are characterized by virtual "micro-communities". As people search for meaningful and personalized communications, interactions are focused on a smaller circle of friends, or people with similar interest networks within social platforms. These virtual networks are represented in a multitude of social networks, including LinkedIn®, Facebook®, SnapChat®, Instagram®, MeetUp® and more. In healthcare, the Patients Like Me® platform provides a series of disease-centric, online communities for people seeking to improve their well-being by sharing common knowledge and experiences. These micro-communities of interest are being used more aggressively by digital marketers to sell products and services, or to drive certain types of behaviors. The trend towards smaller, more intimate and engaged online micro-communities has significant implications for health leaders seeking to build relationships with target audiences, whether it is a consumer or B2B product and/or service offering.
- E = Education. The major elements with Education are: 1) types and level of formal education achieved; 2) health literacy relative to the complexities of medical treatment options and associated costs; and 3) media literacy or how people use technology with a specific focus through the use of mobile apps. Education levels strongly influence employment opportunities, social standing and the types of people within your social network. The educational background sets a framework that can facilitate or deliver barriers to total well-being and improved health status. Formal education levels also affect health literacy levels. Lower health literacy negatively influences the ability to participate in health decisions, whether these are about diet and exercise or a medical procedure.
Media literacy levels directly correlate to how a person uses and benefits from health-related apps and online services. Up to 67% of the U.S. population may currently have a mobile phone, but the key to engaging health-related behaviors is how specific health-related apps are used and leveraged for health improvement. Engaging consumers on all three of these education points requires a high degree of specialization and analysis - no two consumers will necessarily be engaged the same.
The interplay of the various "WE ARE" data-driven SDoH-related dimensions and elements continues to be the subject of many studies and meta-analyses across the industry. Each of these expanding, six areas of DataStreams are driving a revolution in understanding and influencing human health-related behaviors. We include the following case studies as examples.
Healthy Organizations and Communities Apply SDoH and Data to Improve Health
Leaders such as the U.S. Veterans Health Administration and communities throughout the U.S. are integrating SDoH-related data and implementing new data analytics strategies into population health management programs. The following are examples of different strategies and approaches leveraging SDoH-related DataStreams and analytics for overall community health improvement.
Veterans Health Administration (VHA)
The VHA's Office of Health Equity is implementing systems to identify, measure and risk stratify patients by applying and monitoring targeted initiatives. One example is the "Homeless Patient Aligned Care Team"(H-PACT) program, which used data-driven SDoH principles to improve patient care for homeless veterans and their families. These programs are located on the campuses of VA medical centers, community-based outpatient clinics, community resource and referral centers, and co-locate medical staff, social workers, mental health and substance use counselors, nurses, as well as housing placement staff at the facilities.
For this specific population, chronic disease plagues up to 66% and is accompanied by high costs of care. The VHA operated33 H-PACT programs serving thousands of homeless veterans over an 18-month period and conducted a follow-up program assessment. The findings of the H-PACT program are based on a SDoH methodology, and found that population-specific tailoring of clinical care and service delivery were effective in engaging veterans, improving health status and reducing unnecessary acute care use. The high and mid-performing H-PACT sites showed up to a 30% drop in emergency department use, and 20% reduction in hospitalizations. While the program is still ongoing and only in effect since 2012, the premise is based on the central theme that housing availability is a crucial component to overall health.
The Oregon Collaborative
Exactly how to obtain, measure, analyze and apply SDoH-related data across the healthcare system is represented by many evolving processes across the industry's different stakeholder groups - provider, payers, community health clinics. One collaborative example was developed by the Association for Asian Pacific Community Health Centers (AAPCHO), in conjunction with the National Association of Community Health Centers (NACHC), the Oregon Primary Care Association, and the Institute for Alternative Futures. This collaboration piloted a standardized health risk assessment instrument to account for identifying and measuring SDoH factors within specific community populations.
The Protocol for Responding to and Assessing Patients' Assets, Risk and Experiences (toolkit was made publicly available to help a variety of industry stakeholders use best practices, health risk surveys, workflow diagrams and more to develop and implement SDoH-related health improvement interventions. The concept behind this multi-stakeholder pilot is relatively simple - ask a patient about a targeted, measurable list of key factors affecting their life, and incorporate these answers into an actionable care plan. The PRAPARE projects are one example of how a collaboration of different community health stakeholder groups came together to develop and fine tune best practices for identifying and addressing holistic population health needs.
Blue Zones
Blue Zones9 are defined as areas where most people live to the age of 100 years. Through extensive research supported by the National Geographic Society, Blue Zones were identified in specific regions across the globe. These Blue Zones have been identified as: Okinawa, Japan; Sardinia; Italy; the Nicoya peninsula in Costa Rica; and Ikaria, Greece. Typically Blue Zones have been more rural, agricultural regions with a low stress lifestyle and stable relationships. There is one historical Blue Zone region within the U.S. in Loma Linda, California. Loma Linda is a 9,000 person, primarily Seventh-Day Adventist religion-based community featuring the Loma Linda University at its center. This community has broad ethnic backgrounds evolved over time but also has collective population values, norms and characteristics. Studies have shown that the members of this community live as much as a decade longer than the average American citizen. Their longevity can be attributed to vegetarianism, regular exercise, low incidence of smoking and little alcohol use, along with high social connectivity values.
Way to Wellville
The Way to Wellville10 seeks to create Blue Zones in American cities. "Health is an Asset" is the view of the "Way to Wellville" initiative founded by investor Esther Dyson. Typically U.S. citizens assume health until illness strikes. The Way to Wellville is an effort to recreate a Blue Zone in a consumer culture within the U.S. It is starting with five "Wellville" communities that are in the first several years of the initiative. They are: Clapstop County, Oregon; Lake County, California; Muskegon, Michigan; North Hartford, Connecticut; and Spartanburg, South Carolina. These communities are seeking to address the underlying social factors that lead too many citizens to use clinics, emergency rooms, hospitals and pharmacies too much. In essence these communities are incorporating the global strategies of SDoH-driven data, and implementing health improvement plans on a smaller community level.
The City of New Ulm, Minnesota
Started in 2009, Hearts Beat Back: The Heart of New Ulm Project (HONU) is an award-winning population health demonstration project helping people in rural New Ulm, Minnesota, improve their risk factors for heart disease and reduce the total number of heart attacks. As a collaborative research partnership of the Minneapolis Heart Institute Foundation, Allina Health and the New Ulm community, the project has offered a unique environment for studying how various evidence-based interventions, systems and environmental improvements, along with policy changes, can impact the health of an entire community. For the last 10 years, the community of 13,500 has been leveraging the power of SDoH focused data, with a primary focus on changing individual behavior. Critical to the project's success has been engagement with stakeholders in various sectors to utilize data from EHRs, community health screenings, community needs assessments and environmental assessments to assist with engagement, change management, measurement and progress assessment.
The project has delivered evidence-based interventions in a variety of community settings including healthcare, worksites and the broader community. These interventions have spanned a wide gamut - from community health challenges and worksite wellness programs to social marketing campaigns and phone coaching for high-risk patients. Significant shifts have occurred in nutrition programs to support healthier eating and increased physical activity. Examples of these changes include a restaurant program that offers healthier choices; healthier concession choices at sporting events; development of school gardens and a new community co-op facility; more outdoor physical fitness equipment in parks; and Complete Streets-inspired changes to make it safer and easier for people to walk or bicycle.
Health outcome highlights: blood pressure and cholesterol improvements:
- Adults age 40-79 in New Ulm are doing better in controlling their blood pressure, LDL cholesterol, total cholesterol and triglycerides compared to residents in a comparison Minnesota community.11
Five-year project outcomes showed:
- 86% of adults in New Ulm had normal blood pressure, up from 79% in 2009.
- 64% of adults had total cholesterol in the recommended range of under 200, an increase from 59% in 2009.
The percentage of people with their blood glucose under control also increased. From 2008 to 2013, compared with the National Health and Nutrition Examination Survey (NHANES) data, New Ulm's improvements in the above three measures are better than the rest of the country.12
Highlights: nutrition and physical activity improvements
- 33% of people eat five or more servings of fruits and vegetables a day, up from 19% in 2009.3
- 77% now get 150 minutes a week of moderate exercise; up from 67% in 2009.13
The Minneapolis Heart Institute Foundation is finalizing the analysis of the last ten years. As the results become available, the lessons learned will be shared through presentations, papers and consultations. A 20-minute documentary from Health Catalyst on the New Ulm project and the data is available at www.tinyurl.com/NewUlmHealth,and the project's research findings are available at http://heartsbeatback.org/health-leaders/publications.
These efforts from the Veterans Administration to New Ulm are based on understanding how to engage, motivate and support people in shifting from reacting to disease to a proactive, wellness-based culture. Health information across the board has been leveraged to target programs and improve their effectiveness through strategic SDoH data tracking.
"WE ARE" Powers Doing It Better
Health organizations are in the midst of a huge fundamental shift in having data seen as a separate asset and not as an extension of existing health IT systems. Earlier we identified five challenges in integrating the "WE ARE" data sources and insights to transform processes and create new solutions.
- Lack of data leadership and talent can be addressed through new data skills, strategy training programs and implementing new data leadership structures within organizations.
- In order to manage the accelerating data explosion, management needs to begin to understand, analyze and apply the available DataStreams to renovate existing processes, and define the new solutions that are possible.
- Coping with the expanding data velocity depends on building a diverse IT infrastructure to securely support data collection, analytics and storage across all the DataStreams.
- The need to focus on non-medical interventions is critical. The biggest impact on health care costs will come from the application of data-driven SDoH factors as the foundation for catalyzing behavior change in individuals and populations.
Seventy percent of total healthcare costs and health outcomes are determined by SDoH factors and individual behaviors. This article outlined the "WE ARE" approach to harness the power of DataStreams as the vital starting point. Data, like sunshine, is the core source of energy for business. Health data and the associated analytics are being used to prevent readmissions, predict diseases, improve efficiency and invent the future of health.
Creating organizations or communities with a culture of health versus disease is a big challenge. Oregon, the Veterans Administration, New Ulm and other leaders are blazing a trail of "Doing It Better" as they harness the power of data-driven SDoH factors to improve care and outcomes. In today's world a company like Ford is not a car manufacturer, but a "mobility" company. Companies from Merck and Medtronic, to CVS/Aetna, to Amazon/Whole Foods, to Kaiser Permanente and Ascension Health are not just health companies but "life" organizations. When we all do our jobs better with data and health solutions, the people we serve have higher quality and lower costs. And people live better lives. What we do is beyond health - it is about better life.
REFERENCES
- Paul Sawers, "5 billion people now have a mobile phone connection, according to GSMA data", 2017, https://venturebeat.com/2017/06/13/5-billion-people-now-have-a-mobile-phone-connection-according-to-gsma-data/, (Accessed March 15, 2018).
- U.S. Centers for Disease Control, "Sources for Data on SDOH", (https://www.cdc.gov/socialdeterminants/data/index.htm), (Accessed March 20, 2018).
- U.S. Centers for Disease Control, "Data Set Directory", (https://www.cdc.gov/dhdsp/docs/data_set_directory.pdf/, (Accessed April 10, 2018).
- U.S. Centers for Medicare and Medicaid Services, Press Release, ((https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2018-Fact-sheets-items/2018-03-06.html), (Accessed April 14, 2018).
- Amazon Web Services, (http://aws.amazon.com/datasets), (Accessed April 10, 2018).
- Google, (https://www.google.com/publicdata/), (Accessed April 9, 2018).
- U.S. Office of Disease Prevention and Promotion, (https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health), (Accessed April 10, 2018).
- National Association of Community Health Centers, PRAPARE Implementation and Toolkit, (www.nachc.org/research-and-data/prapare/), (Accessed April 10, 2018).
- Blue Zones Project, (https://www.bluezonesproject.com/), (Accessed April 10, 2018).
- HICCup (Health Initiative Coordinating Council, 2018, (www.wellville.net/about-wellville/), (Accessed April 15, 2018).
- Assessing the Impact of The Heart of New Ulm Project: A Population-Based Program to Reduce Cardiovascular Disease, a presentation at the American Heart Association EPI/Lifestyle 2017 Scientific Sessions.
- Changes in cardiovascular risk factors after 5 years of implementation of a population-based program to reduce cardiovascular disease: The Heart of New Ulm Project. American Heart Journal 2016, DOI: 10.1016/j.ahj.2016. 2.006.
- New Ulm community heart health screening data.
- Login to post comments