 Just a few years ago, things were looking up for the American health care system. We were going to start finding better ways to pay for care: call it pay-for-performance (P4P), value-based purchasing (VBP), or similar terms. We were going to nudge -- or, rather, push -- providers into more clinically integrated systems (e.g., ACOs) to help improve outcomes and to control costs. And, of course, with wider use of electronic health records (EHR), we'd be able to better coordinate care and make decisions based on actual data. It all sounded very promising. Now, though -- what's that old expression about the leopard not being able to change its spots?...
Just a few years ago, things were looking up for the American health care system. We were going to start finding better ways to pay for care: call it pay-for-performance (P4P), value-based purchasing (VBP), or similar terms. We were going to nudge -- or, rather, push -- providers into more clinically integrated systems (e.g., ACOs) to help improve outcomes and to control costs. And, of course, with wider use of electronic health records (EHR), we'd be able to better coordinate care and make decisions based on actual data. It all sounded very promising. Now, though -- what's that old expression about the leopard not being able to change its spots?...
 At this year’s HIMSS conference, interoperability was again one of the hottest topics of discussion. Interoperability was even a featured showcase at the HIMSS Interoperability Showcase. Yet the lack of interoperability in HealthIT remains. "HealthIT is not unique in its interoperability woes and other industries, including the automotive industry, are still struggling with associated safety issues."
At this year’s HIMSS conference, interoperability was again one of the hottest topics of discussion. Interoperability was even a featured showcase at the HIMSS Interoperability Showcase. Yet the lack of interoperability in HealthIT remains. "HealthIT is not unique in its interoperability woes and other industries, including the automotive industry, are still struggling with associated safety issues."
 In an article published in JMIR Medical Informatics, researchers from the University of California-Davis decided to explore the small but intriguing world of open source EHRs, which may fit very neatly into the growing interest in application programming interfaces, FHIR, and other open data standards that encourage customized mix-and-match health IT development without the historical pitfalls of proprietary systems. Using data from 2014, the researchers identified 54 open source projects that met the HHS definition of an electronic health record. At the time, four of those packages had achieved Certified EHR Technology status from the ONC.
In an article published in JMIR Medical Informatics, researchers from the University of California-Davis decided to explore the small but intriguing world of open source EHRs, which may fit very neatly into the growing interest in application programming interfaces, FHIR, and other open data standards that encourage customized mix-and-match health IT development without the historical pitfalls of proprietary systems. Using data from 2014, the researchers identified 54 open source projects that met the HHS definition of an electronic health record. At the time, four of those packages had achieved Certified EHR Technology status from the ONC. Healthcare applications face different challenges than their counterpart in consumer applications. They are not designed to replace providers or to improve the efficiency and scalability of providers. EMR and EHR systems have common characteristics with a database system, but they are designed for healthcare. In other words, healthcare needs its own stack. Healthcare middleware must address all the common services required to support application development. Having a set of APIs access EMR and EHR systems is the starting point, but not the complete solution. Messaging, workflow, rule engine services, and more must be part of a middleware solution. Its footprint must be lightweight and cost efficient so that it can be embedded with the applications. The real healthcare challenge is addressing the missing healthcare applications in support of a diverse care environment. Our efforts must align to inspire developers in addressing providers’ needs. It will be healthcare applications that will evolve healthcare to the next level.
Healthcare applications face different challenges than their counterpart in consumer applications. They are not designed to replace providers or to improve the efficiency and scalability of providers. EMR and EHR systems have common characteristics with a database system, but they are designed for healthcare. In other words, healthcare needs its own stack. Healthcare middleware must address all the common services required to support application development. Having a set of APIs access EMR and EHR systems is the starting point, but not the complete solution. Messaging, workflow, rule engine services, and more must be part of a middleware solution. Its footprint must be lightweight and cost efficient so that it can be embedded with the applications. The real healthcare challenge is addressing the missing healthcare applications in support of a diverse care environment. Our efforts must align to inspire developers in addressing providers’ needs. It will be healthcare applications that will evolve healthcare to the next level. Our relationship with technology is not unidirectional. We use it, and it changes us. But it cannot alter fundamental realities regardless of how hopeful Americans are or how much faith we have in it. More and better technology is not a substitute for adequate funding and coordinated planning, especially when we’re talking about the very significant funding issues around behavioral health. Sure, we can get excited about the newest app and the latest EHR functionality, but we must also maintain a focus on meeting the needs of the mental health professionals committed to keeping our fellow citizens from falling through the cracks. Even while there is no magic in technology, there is also no reason to believe we can’t fix a broken mental health system through hard work, empathy and thoughtful planning. Time and again, our faith in those principles has been rewarded.
Our relationship with technology is not unidirectional. We use it, and it changes us. But it cannot alter fundamental realities regardless of how hopeful Americans are or how much faith we have in it. More and better technology is not a substitute for adequate funding and coordinated planning, especially when we’re talking about the very significant funding issues around behavioral health. Sure, we can get excited about the newest app and the latest EHR functionality, but we must also maintain a focus on meeting the needs of the mental health professionals committed to keeping our fellow citizens from falling through the cracks. Even while there is no magic in technology, there is also no reason to believe we can’t fix a broken mental health system through hard work, empathy and thoughtful planning. Time and again, our faith in those principles has been rewarded.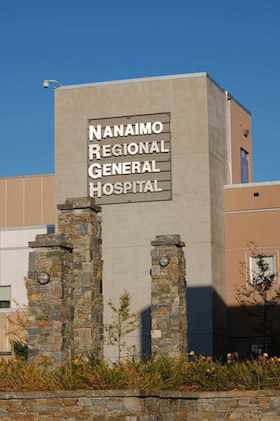 Vancouver Island Health Authority in British Columbia, Canada, is in the midst of rolling out Cerner's EHR across its system, but physicians are petitioning to suspend the go-live, citing concerns regarding patient safety, according to a Times Colonist report. In 2013, Island Health signed a 10-year, $50 million deal with Cerner to implement the EHR across the system, which includes an additional $124 million for hardware and training. The EHR went live at Nanaimo Regional General Hospital, a residential care center and another health center on March 19...
Vancouver Island Health Authority in British Columbia, Canada, is in the midst of rolling out Cerner's EHR across its system, but physicians are petitioning to suspend the go-live, citing concerns regarding patient safety, according to a Times Colonist report. In 2013, Island Health signed a 10-year, $50 million deal with Cerner to implement the EHR across the system, which includes an additional $124 million for hardware and training. The EHR went live at Nanaimo Regional General Hospital, a residential care center and another health center on March 19... CommonWell Health Alliance and Carequality announced today an agreement to increase health IT connectivity nationwide. The agreement provides additional health data sharing options to a broad range of stakeholders across healthcare, and has three aspects:
CommonWell Health Alliance and Carequality announced today an agreement to increase health IT connectivity nationwide. The agreement provides additional health data sharing options to a broad range of stakeholders across healthcare, and has three aspects: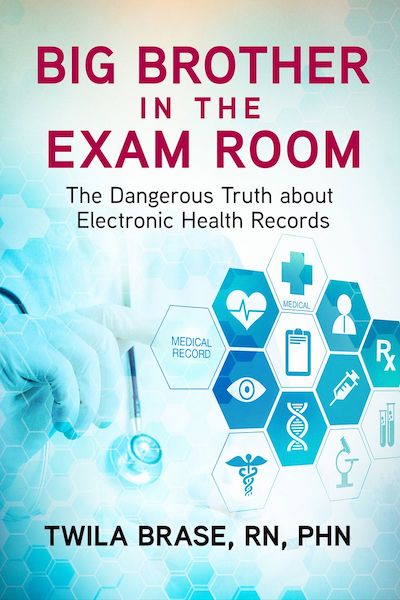 A new, groundbreaking book from Citizens’ Council for Health Freedom (CCHF) will expose how the mandated, government-certified EHR technology (CEHRT) has negatively affected both doctors and patients. Written by CCHF president and co-founder Twila Brase, RN, PHN, and published by Beaver’s Pond Press...Brase’s extensively researched work shows how and why Congress forced doctors and hospitals to install a data-collecting, command and control surveillance system in the exam room. It also includes the impact of EHRs on privacy, patient care, costs, patient safety and more, according to doctors and more than 125 studies....This week, Brase is unveiling “Big Brother in the Exam Room” at FreedomFest 2018 at the Paris Resort Las Vegas. Brase will be a part of several panels and will introduce the book to fellow freedom-loving patriots who recognize that rights also extend to health care...
A new, groundbreaking book from Citizens’ Council for Health Freedom (CCHF) will expose how the mandated, government-certified EHR technology (CEHRT) has negatively affected both doctors and patients. Written by CCHF president and co-founder Twila Brase, RN, PHN, and published by Beaver’s Pond Press...Brase’s extensively researched work shows how and why Congress forced doctors and hospitals to install a data-collecting, command and control surveillance system in the exam room. It also includes the impact of EHRs on privacy, patient care, costs, patient safety and more, according to doctors and more than 125 studies....This week, Brase is unveiling “Big Brother in the Exam Room” at FreedomFest 2018 at the Paris Resort Las Vegas. Brase will be a part of several panels and will introduce the book to fellow freedom-loving patriots who recognize that rights also extend to health care...