American Medical Association’s Problem with the Lack of EHR Usability
 Shameem C. HameedEarlier this week Joe Conn, reporter for Modern Healthcare, broke the story that the American Medical Association (AMA) and 34 other medical specialty societies and organizations had sent a 9-page scathing letter to the Office of the National Coordinator for Health Information Technology (ONC) demanding a major overhaul of the government’s electronic health record (EHR) policies. According to Conn:
Shameem C. HameedEarlier this week Joe Conn, reporter for Modern Healthcare, broke the story that the American Medical Association (AMA) and 34 other medical specialty societies and organizations had sent a 9-page scathing letter to the Office of the National Coordinator for Health Information Technology (ONC) demanding a major overhaul of the government’s electronic health record (EHR) policies. According to Conn:
“The American Medical Association is calling for an overhaul of a federal program to test and certify electronic health-record systems for suitability in the EHR incentive-payment program. Its request has been joined by 34 other medical specialty societies and healthcare professional organizations.
‘We believe there is an urgent need to change the current certification program to better align end-to-end testing to focus on EHR usability, interoperability and safety,’ the group said. ‘Physician informaticists and vendors have reported to us that MU (meaningful use) certification has become the priority in health information technology design at the expense of meeting physician customers' needs, patient safety and product innovation.’
A 9-page letter to the head of the Office of the National Coordinator for Health Information Technology (PDF) complained of “documented challenges and (a) growing frustration with the way EHRs are performing.” Such problems are inadequately addressed by the federal EHR testing and certification program led by the ONC, the AMA and its colleagues contend.”
There it is--an official validation to my argument that there is a need for a highly customizable EHR. I never get tired of this quote from Dr. Lawrence Hoffman: “EHRs are like the Model-T, any color as long as it is black.” One of the key complains that the 35 medical organizations are making is the lack of adaptability and customizability of current EHR systems. They are saying that an EHR is used in different ways in different environments, such as in acute care and ambulatory settings. My argument goest beyond that of the AMA...EHRs are used by each specialty and each individual doctor within a specialty in different ways as well.
Usability
One major gripe of the AMA is the lack of usability of most EHR systems. If you look at many of the EHR systems in the market today, they feel like the cockpit of a 747 Jumbo jet, clunky and intimidating. Very few EHR system vendors have thought about the interfaces in a deeper level. Some EHR vendors think that by taking away features from the EHR they will make them simple to use. However, that means that their EHR remains a one trick pony that can be used by what they call “a single provider” practice. In reality, even those providers using the “simplified” EHRs put up with them for lack of a better choice.
 Design principles that must be employed in EHR systems are in a different category altogether than those of other systems. Understanding the nature of how a system is used is important. The kinds of questions one has to ask, for example, include how long will someone be using this system? And, what are they going to use it for? These kinds of applications are used for a longer period continuously than say, a shopping web site. So would the same principles be applicable? The flow of the EHR should follow the thought process of a doctor, not the other way around where the doctor has to follow the flow of the EHR. However simple or beautiful the app is, if it is designed for the wrong user and use, it will not work efficiently.
Design principles that must be employed in EHR systems are in a different category altogether than those of other systems. Understanding the nature of how a system is used is important. The kinds of questions one has to ask, for example, include how long will someone be using this system? And, what are they going to use it for? These kinds of applications are used for a longer period continuously than say, a shopping web site. So would the same principles be applicable? The flow of the EHR should follow the thought process of a doctor, not the other way around where the doctor has to follow the flow of the EHR. However simple or beautiful the app is, if it is designed for the wrong user and use, it will not work efficiently.
Even if EHR vendors failed to do usability research on how best to design a good medical software interface, some basic principles can be followed. At ZH Healthcare we have made usability the core of our EHRs and personal health record (PHR). An example of a design concept that we followed is to bold the data-fields rather than the label fields. Sounds simple, but when you think about it, it makes sense. If you, as a doctor, are looking at the EHR screen all the time in your practice, you know where the label “Sex” or “Name” is. You don’t need to see the labels in bold all the time: that is not what should catch your attention. You need to see the data in bold so that you can glance at it once.
How many doctors ask their patients to come on a certain date? Not many. Doctors generally use time frames like “see me in a week, or in a month.” This concept is lacking in the current crop of EHR systems. The placement and color coding of allergy information, the display of appointments, are all simple but key issues that need to be concentrated on.
We went through multiple researches by acknowledged organizations and universities to include the latest design principles in the development of our cloud-based BlueEHS electronic health system. In addition, as an open source EHR developer, we received an enormous amount of feedback from our open source community of doctors and other medical practitioners.
Forms
The next major gripe of the AMA and 34 other medical organizations, is about the inflexibility of the systems. When EHR systems talk about “customizable” or “flexible,” what they mean is you can make your own forms using a tool that allows you to add fields. That is it, you are supposed to be happy.
Each doctor uses his own unique set of forms that he might have tweaked to his satisfaction over the years. This doctor should be allowed to use those form while transferring to an electronic health records system. These forms could contain check boxes, note boxes, radio buttons, selection lists, and even images that can be marked up. He should be able to input data either by typing, scribbling on a pad, or voice to text or just record his voice for transcribers.
Now enhance it another level. Say you are a large practice with 15 different specialties and 40 providers in multiple locations in different time zones. So how are you going to have all these different set of forms in a single EHR if all they allow you to do is tweak some static form?
The letter by the AMA continues to say,“We believe there is an urgent need to change the current certification program to better align end-to-end testing to focus on EHR usability, interoperability and safety,” the medical groups said. “Physician informaticists and vendors have reported to us that MU (meaningful use) certification has become the priority in health information technology design at the expense of meeting physician customers’ needs, patient safety and product innovation.” MU certification alone was the goal of all the leading proprietary EHR companies.
In sharp contrast, developers of open source EHRs have focused on usability and interoperability from the beginning. For example, take a look at the BlueEHS WYSIWYG (what you see is what you get) form builder to see the power of building your own form without the help of a “techie.”
 Workflow
Workflow
Unit testing “does little to assure a product’s performance once deployed in a clinical environment,” the AMA group wrote. Instead, the AMA and the others said EHRs should be rigorously tested “against a multitude of clinical scenarios that represent the variety of workflows seen in acute and ambulatory care settings.” This is where most, if not all, proprietary EHR companies fail. They all have one workflow for every office. Many do not even have a treatment plan, let alone a workflow designer.
So what is a treatment plan? It is a set of actions at a defined period of time to meet a particular objective as it relates to the treatment of a patient. One should be able to track the progress of the plan and tweak it and alter it as one goes along. Rigidity is anathema in this case. This is specially important in the age of personalized medicine where the doctor must have the ability to allocate a treatment plan for each individual patient. Proprietary EHR systems that claim they have a treatment plan do not usually have patient specific plan. Case management and tracking must also follow this process.
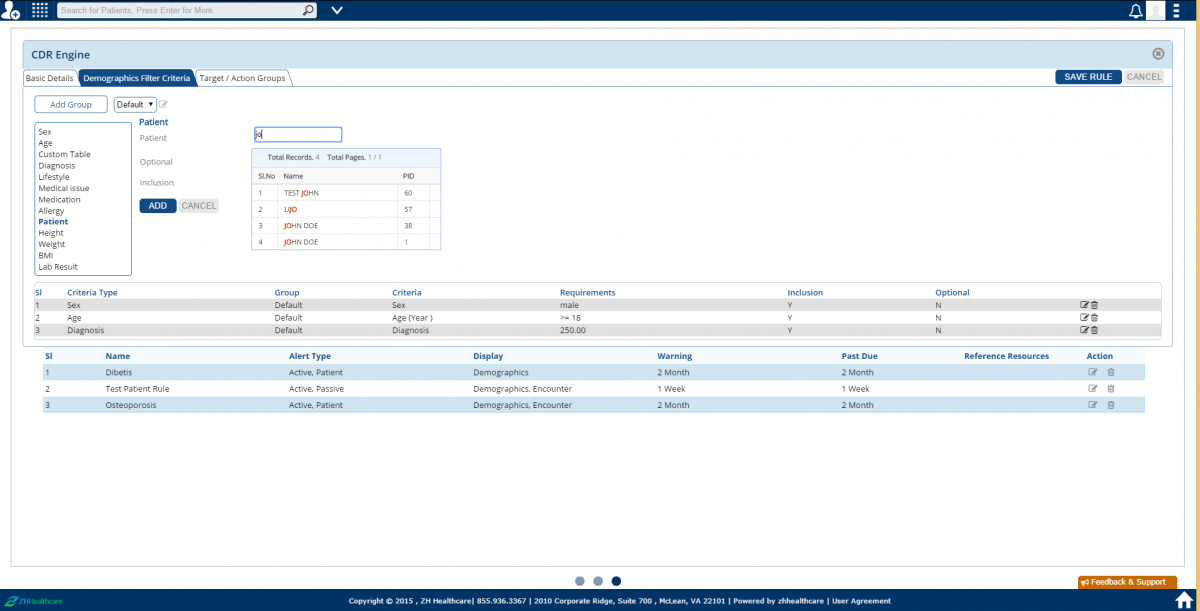
Workflow relates to the practice. How they see a patient and how the process is handled in a clinical environment is key. Proprietary EHR vendors don’t think of adding a flexible workflow into the EHR system because they don’t see the EHR as an Electronic Health Solution, but just a place to store Electronic Health Records. A sort of digital filing cabinet if you will. The image above shows how BlueEHS uses its CDR engine tool to build a treatment plan and a workflow.
Many practices and organizations have found their answer to these problems by adopting any one of several excellent open source EHRs that are superior in every respect to the proprietary EHRs that the AMA is criticizing. The VA’s open source VistA EHR, for example, is an excellent choice for hospitals and large-scale health systems. As this article details, VistA is hands down the best option to replace the current EHRs used by the US Department of Defense. For clinics and physician offices, our very own BlueEHS, offers a good a hybrid open source alternative. It could have been Einstein who said “If you can’t explain it to a six year old, you don’t understand it yourself.” I would say that is what the EHR system should do, present the highly complicated world of digital health to the end user in a way that they can use it cognitively and intuitively.
Updates
2/3/2015 - Added workflow image.
- Tags:
- American Medical Association (AMA)
- BlueEHS
- case management
- EHR interoperability
- EHR safety
- EHR usability
- Electronic Health Record (EHR)
- electronic health system (EHS)
- health information technology (HIT)
- human factor engineering (HFE)
- Joe Conn
- Lawrence Hoffman
- Meaningful Use (MU)
- Modern Healthcare
- MU certification
- Office of the National Coordinator for Health Information Technology (ONC)
- open source EHR
- personal health record (PHR)
- personalized medicine
- Physician informaticists
- Shameem Hameed
- US Department of Defense (DoD)
- usability research
- VistA EHR
- ZH Healthcare
- Login to post comments