White Paper: Stop the Referral Problem - Building Digital Care Transitions that Reach Your Entire Network
 Catherine ThomasThe healthcare industry has crossed a digital chasm-at least in part. Patient records have moved from paper to computer and many transactions, such as e-prescribing and lab orders have been automated, to accelerate workflows, minimize mistakes and reduce costs. But when it comes to sharing patient records, especially beyond the four walls of a hospital, we remain in the dark ages of paper and fax.
Catherine ThomasThe healthcare industry has crossed a digital chasm-at least in part. Patient records have moved from paper to computer and many transactions, such as e-prescribing and lab orders have been automated, to accelerate workflows, minimize mistakes and reduce costs. But when it comes to sharing patient records, especially beyond the four walls of a hospital, we remain in the dark ages of paper and fax.
Referrals and other transitions in care, transactions that require the careful handoff of patient information to another member of their care team, are largely done the same way that they were before the move to electronic medical records. Communications are one-way, with little expectation of feedback, and information typically has to be manually entered into the receiving party's EHR, if at all. This is labor-intensive, expensive, and diminishes the ROI of using electronic records in the first place. Data that starts out digitally should remain digital, and the industry should leverage information technology to manage workflows rather than relying so heavily on overworked clinical staff. According to IDC Health Insights' Healthcare Provider Survey in 2015[i], the top three most common ways of sending and receiving patient information were paper, phone, and fax:
In this paper, we will discuss our research about how referrals and care transitions are typically conducted; the financial, non-financial, and quality impacts on patient care; and near-term opportunities for leveraging technology to accelerate these processes to benefit provider organizations and to deliver a high-quality, efficient patient experience.
 Source Data - IDC Healthcare Provider Survey, January 2015
Source Data - IDC Healthcare Provider Survey, January 2015
Gaps and Inefficiencies in Patient Care Transitions
Many of us have experienced inefficient care transitions from the patient or caregiver perspective, but what is truly happening in the provider setting? Interviews with hundreds of clinical staff have identified five dominant challenges for hospitals and the healthcare providers they interface with:
1. Care Transitions are Communication Workflows, But Most Are Not Managed That Way
EHRs are strong at capturing data, managing internal orders, and capturing billing information, but they have not been designed to manage the clinical workflows required to coordinate patient care beyond the "four walls" of the hospital.
To address these limitations, many organizations have implemented portals or participate in Health Information Exchanges (HIEs) to provide data access to outside providers. However, this typically requires the provider to login and "pull" data and often lacks substantive patient record details such as provider notes, studies or image files. Even when the provider receives Admission, Discharge, and Transfer (ADT) alerts from the hospital, and can pull the patient's record from an HIE or portal, it is not typically sufficient for an effective referral, for discharging the patient into the care of their PCP, or transferring a patient to the care of a Skilled Nursing Facility (SNF).
Why? Because in addition to the structured patient data, a healthcare system relies on "knowledge workers" who need to interact with each other to efficiently learn and convey information about a mutual patient. These clinical communications are nuanced so, in addition to having access to the patient data, they need a two-way dialogue about the subjective nature and specific details of a patient's care. These needs have kept providers on the telephone and fax machine, with 63% continuing to rely on fax as their primary method of sharing patient information[ii].
2. Fax is Not Digital
Fax has several limitations that keep it from being viable in the long run if healthcare is to become a credible digital industry:
- Patient Records received via fax are not "searchable" by the receiving provider. Looking for a cholesterol or glucose value or the presence or absence of a previous test or study means a person must scan or read the entire analog fax record.
- Faxed records cannot be integrated into the structured portion of the patient record. For example, faxed lab values from one facility cannot be imported and easily compared with related values already stored in the EHR to present a graph over time. Even if the fax is scanned and uploaded to the record, important data needs to be sought out and can easily be overlooked. This often leads to errors of omission and reduces the effectiveness of alerts for conflicts such as problematic medication dosing or interactions.
- Since faxes cannot be imported to the structured fields in the receiving EHR, administrative support teams routinely need to re-enter selected patient data. This adds to organizational inefficiency and often results in transcription errors.
- And, since fax is one-way, it lacks built-in workflow to close feedback loops and has no convenient mechanism for follow-up discussion.
3. Telephone is Not Digital Either
Because Physicians work best when they can ask questions and get clarification from other clinicians, real-time voice conversations are extremely important in the practice of real-world healthcare. But simply arranging for two busy clinicians to talk is very difficult; and even more so if they work for different organizations or need to involve additional members of a dispersed care team. The inability to easily coordinate these types of calls frequently leads to no communication at all. Moreover, real-time conversations via phone, video or other technologies are not captured in ways that can be readily delivered into a patient medical record to assist clinical or administrative functions.
Other industries have long since complimented real-time conversation with digital tools that allow for active collaboration. Store-and-forward systems like email, near-real-time communications like texting, and other collaboration systems dominate most other industries. They not only support query methods and help with prioritization, alerting and subtlety, but they are very efficient because they work well asynchronously and at any distance, allowing people to communicate in bursts during idle moments whether the others are available or not.
4. Lack of Readily Available, Trusted and Detailed Clinician Directories
According to the American Medical Association, there are more than 814,000 active U.S. physicians, 2.8M nurses and over 5M clinical staff. When including public health workers, community health aides, home health workers, and others, the numbers only increase. How can we coordinate care across a patient care team without easy ways to find and reach all of them?
The Direct protocol was designed to provide a safe mechanism for one clinician exchanging messages with another but there are only 587,000 addresses listed in the DirectTrust directory[iii]. When you consider the 5M clinical staff and millions of additional support staff, direct reaches only a small proportion of the audience and therefore cannot be widely relied upon for referrals and transitions in care. And a solution that reaches only a fraction of healthcare providers is no solution at all.
5. Referral and Care Transition Processes are Labor-Intensive
A typical referral is handled by 5 or more people and takes about 20 steps to complete. And this is just the portion that involves getting a referral to the other provider and not requests for more information or feedback to the sender. Involving so many people can easily delay delivery and impact patient care. In fact, if a discharge summary is delayed 3 days, it can cause up to a 10% increase in a hospital's 30-day readmission rate.[iv]
At the receiving end, specialists frequently want more information than is contained in the original referral and they want a dialogue. In a recent study, the additional information most often requested was the problem to be addressed (53%), further patient history (41%), and a chance to ask questions of the PCP before seeing the patient (35%)[v]. In the same study, the referring doctor, only received feedback from the specialist 50% of the time, and in our experience, this is optimistic.
Workflow Use Case: FQHC to a Hospital Referral
In an inpatient setting, when a physician, or nurse or other clinical worker goes off duty there is a routine, but well-orchestrated handoff to the next clinician. Some call it rounds, a briefing, or the "bullet". With complex cases, this handoff takes more time and is carefully managed. A similar approach is used when a patient is transferred from one ward or unit to another. In most cases there is a dialogue involving a briefing with questions and answers and recommendations. The practice of relying entirely on the information in the patient's EHR is rare.
Why is the handoff associated with a referral or a transition in care so different? In theory, it shouldn't be different at all. At a high-level, a well-managed handoff should include:
- A way of finding and reaching the recipient-including the identification of preferred providers to prevent referral leakage
- A narrative description of the patient's condition, history and reasons for referral or transition
- The appropriate parts of the patient's record in a format that can be uploaded into the recipient's EHR
- A fast and efficient way to allow the recipient to ask questions or request missing data
- A mechanism for the sender to track the patient's progress (including scheduling, attendance and treatment updates)
- Feedback to the referring party at the conclusion of the encounter(s), ideally in a form that can be part of the EHR for both parties.
When any of these components are not working efficiently or are error-prone, the patient AND clinician experiences both suffer, costs rise, and patients may struggle to get the right care when they need it. The flowchart below, is typical of a 20-step referral process from a Federally Qualified Health Center (FQHC) to a hospital specialist.[vi].
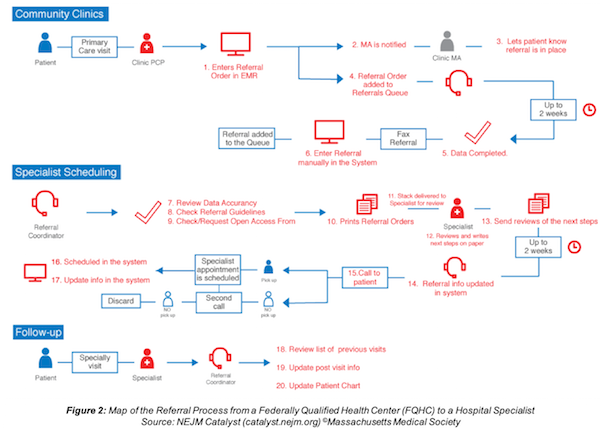 Figure 2 - Map of the Referral Process from a Federally Qualified Health Center (FQHC) to a Hospital Specialist Source - NEJM Catalyst (catalyst.nejm.org) ©Massachusetts Medical Society
Figure 2 - Map of the Referral Process from a Federally Qualified Health Center (FQHC) to a Hospital Specialist Source - NEJM Catalyst (catalyst.nejm.org) ©Massachusetts Medical Society
From the flow chart, it is clear that a typical referral process is time-consuming, paper-driven, and reliant on multiple touches from providers and support teams on both sides of the process to ensure completion. There are two incidences of 2-weeks delays, and several references each to manual data entry, faxing, printing, phone calls and other labor-intensive tasks.
The Real Costs of Inefficient Care Transitions
Now let's consider the financial and non-financial impacts on both healthcare providers and patients with these incomplete, manual referral and care transition processes, including:
1. Operational Costs - Many industries need to look far in the past to recall the days of high paper and printing costs, but in healthcare, this remains a reality. But the challenges remain even when paper and ink is not used. E-faxing services have reduced some of those costs but have not removed the heavy administrative toll on personnel who are manually uploading and renaming files, reading content, and often times re-entering the same patient data that was collected during a previous encounter. Even within a single health system, multiple people often enter the SAME data, wasting valuable resources and adding time to each step of the process.
2. Referral Leakage - When persistent out-of-network referrals occur, hospital systems and accountable care organizations lose the associated revenue of providing follow-up care within their primary, specialty, or other post-acute care service areas, so they have a significant incentive to provide the tools, such as comprehensive clinician directories, to help their providers refer to the network of providers that makes the most sense. Similarly, hospitals have an incentive to form strong relationships with community doctors to drive inbound referrals and to safely hand-off a patient's care post-discharge. And patients suffer too, because tests need to be repeated, more errors occur, and coordination suffers.
3. CMS Reimbursements - Beginning in 2019, the Centers for Medicare and Medicaid Services will require hospitals and practices to begin sharing patient records electronically when referring or transitioning a patient to another organization. The economic incentives from this program (known as "Promoting Interoperability") are significant, with penalties equal to 2-7% of CMS reimbursements if they fail to comply. And alongside the new "PI" guidelines will be increasing enforcement of information blocking policies, so hospitals have a large financial incentive to take the reins of how and when they share digital information to ensure compliance.
4. Lack of Feedback Loops - A "feedback loop" is completed when the originator of a referral receives timely and meaningful feedback about his/her patient's care. Given the prevalence of fax, and a lack of digital options to easily and cost-effectively communicate throughout the referral process, many providers are left without information about the care a patient has received. This can cause several negative impacts on care quality, including:
- Unnecessarily repeated patient tests due to limited secure file sharing capabilities and ad-hoc communication channels for providers, especially for those in separate provider organizations.
- Increased risk of Medical errors due to lack of awareness of current medications, allergies, care plans, etc. As of 2012, 80% of all serious medical errors involved miscommunication during care transitions[vii].
- Increased risk of hospital readmission due to poor communication and awareness of the subtleties and priorities about patient conditions or hospitalization.
- Reduced patient care coordination, with particular ongoing impact for patients with chronic conditions and the providers working to improve outcomes and gain reimbursement under value-based care models.
5. Patient Satisfaction - At the center of the care team is the patient. Their experience determines whether they return to a given provider, how they rate providers, and how the quality of care impacts their overall health. When navigating between providers, patients expect that the person they are being referred or transitioned to knows their medical history, and that feedback will be sent to the referring doctor (often primary care) so that ongoing care considers the results from the referral. Patients are often sadly disappointed and frustrated when these basics are missed.
Opportunities for Improvement TODAY
There is no doubt that healthcare has a herculean task to solve the referral and transition in care challenge. Many hospitals and small providers are cash-strapped or addressing other critical areas such as patient safety, expanding patient access to providers via telehealth programs, and other valuable initiatives. But this is the digital age, in which many companies are growing and thriving by quickly and securely sharing data. Beginning today, hospitals should consider implementing tools to do the following:
1. Publish national and organization directories so providers can reach each other. Doing this will improve a hospital's and practice's ability to reduce referral leakage & inappropriate referrals by empowering providers to refer to the "right" specialist for a particular patient and begin to build trust in the referral network. Directories can also yield these benefits:
- Help discharge coordinators identify specialists that are convenient for a patient, based on location or accepted insurance, for example.
- Better align provider specialty and subspecialty with a patient's needs, reducing the risk of re-referrals or the patient independently leaving the network due to dissatisfaction.
2. Share referrals and other care transitions digitally, attaching a copy of the patient's medical record in a format that can be uploaded or digitally available to the recipient's EHR. Not only will this keep the patient's health history digital and searchable, and allow for other automation, but it will significantly reduce duplicate data-entry, scanning/faxing/printing at the receiving end, improve patient data quality at the point-of-care, and reduce burden on the patient to carry information.
Once the patient encounter is complete at the receiving end, hospitals can close referral feedback loops. Creating (and closing) electronic referral loops is an important requirement in the Promoting Interoperability program and digital information can also be efficiently added to the patient record at either end.
3. Enroll in a service that allows for digital communications with any healthcare provider - not just those with the same EHR or with a Direct protocol address. Many hospitals have selected internal texting or secure email capabilities; many are using HIEs to share information with a small group of other facilities; and many are working with EHR vendors to expand their toolkits. But these are unfortunately only partial solutions, and do not broadly engage with the entire care community to embrace the fact that patients seek care in a variety of settings, both inside and outside of a hospital or system and with providers big and small.
Conclusion
The digital era of healthcare is upon us. Hospitals have implemented and thoroughly embedded EHRs into their operations and should now maximize that investment by making good on the promise of patient data exchange. As we have learned, referrals and care transitions are not working efficiently in most cases, HIEs and EHR-specific portals have helped but are not nationally available solutions and lack key capabilities, technology protocols such as Direct have not achieved broad adoption, and many other challenges persist.
Hospitals and their physician networks should now seek specialized solutions that solve issues such as a) finding any provider recipient, b) sending digital patient information electronically and enabling feedback loops, and c) delivering tools and workflows that align with the facility's needs.
Secure tools, such as careMESH, are available in the market today, and are capable of integrating with almost any EHR to drive referral efficiency and reduce burden on clinical and administrative staff. With these new technology options, providers can now:
- Dramatically reduce the use of printing, scanning, and fax
- Eliminate duplicate data entry and the corresponding burden on administrative staff
- Create digital feedback loops to meet Promoting Interoperability requirements, and
- Embed a secure channel for ad-hoc communications and updates throughout the process
And with built-in identity proofing, secure messaging, a national clinician directory, a universal patient record viewer, and national reach, careMESH makes it possible for hospitals and practices to collaborate better than ever before.
[i] https://www.healthpopuli.com/2016/04/11/not-sharing-patient-health-data-threatens-health/
[ii] https://www.healthcareitnews.com/encrypted-fax-over-cloud-network
[iii] https://www.directtrust.org/
[iv] https://www.journalofhospitalmedicine.com/jhospmed/article/127420/discharge-summaries-and-readmissions#
[v] https://www.ncbi.nlm.nih.gov/books/NBK43671/
[vi] https://catalyst.nejm.org/econsults-save-medicaid-referrals/
[vii] https://www.jointcommission.org/assets/1/6/tst_hoc_persp_08_12.pdf
- Tags:
- care coordination
- careMESH
- Catherine Thomas
- Centers for Medicare and Medicaid Services (CMS)
- CERHT-compliant EHR
- clinician directories
- cloud-based communications platform
- digital care transitions
- digital referrals
- Direct protocol
- discharge coordinators
- Electronic Health Record (EHR)
- electronic medical records (EMRs)
- fax machines
- Federally Qualified Health Center (FQHC)
- Health Information Exchange (HIE)
- healthcare industry
- Healthcelerate
- IDC Health Insights' Healthcare Provider Survey
- Meaningful Use
- Medicaid EHR Incentive Program
- medical errors
- MU-2 HIE
- patient data exchange
- patient record
- Peter Tippet
- Promoting Interoperability
- structured medical record
- transitions of care
- White Paper
- Login to post comments